Lupine Publishers | Journal of Otolaryngology
Background: Allergic rhinitis (AR) is characterized by
inflammation in the nose as the immune system respond to inhaled
allergens in the air. Signs and symptoms include a runny, stuffy red and
itchy nose, sneezing with watery eyes, and swelling around
the eyes A deviated septum mostly is asymptomatic, but sometimes may be
presented by difficulty breathing through the nose, nasal
congestion, sinus infections, nosebleeds, sleep apnea, headache, and
postnasal drip. Septoplasty is the main surgical intervention for
patients with deviated nasal septum to relieve nasal obstruction. While
Allergic rhinitis is mainly treated with anti-allergy medicine.
Aim: To detect the incidence of post-septoplasty complications among patients with deviated nasal septum and Identify the
correlation between the allergic rhinitis and post-operative complications as compared with non-allergic patients.
Methodology: A retrospective Electronic record-based study was conducted including all patients with clinically diagnosed as
deviated nasal septum and undergone surgical intervention at Khamis Mushait General Hospital. Data extracted included patient’s
demographic data, recorded post-operative complications and history of having allergic rhinitis.
Results: The study included a total sample of 93 patients;
Nasal obstruction was the most frequent complaint among patients.
As for post-operative complications, nearly one third of the cases had
nasal obstruction followed by external nasal deformity, and
smell disturbance. Nasal obstruction was diagnosed higher among patients
with allergic rhinitis (P=.142). External nasal deformity
was recorded among 6.2% of the cases with allergic rhinitis compared to
3.6% of others without allergic rhinitis. Regarding smell
disturbance, it was reported among 13.8% of the patients with allergic
rhinitis compared to 3.6% of those without allergic rhinitis.
Conclusions: The study revealed that post-septoplasty nasal
obstruction as a complication is most common with similar
incidence rate in both allergic and non-allergic rhinitis patient groups
while septal hematoma was least common. All post septoplasty
complications except nasal obstruction were found to be significantly
higher among allergic rhinitis cases.
Keywords: Allergic rhinitis, septoplasty, surgical intervention, deviated septum, complications, nasal allergy
Abbreviations: DNS: Deviated Nasal Septum; AR: Allergic Rhinitis; CSF: Cerebrospinal Fluid
Introduction
Allergic rhinitis (AR) is a prevalent disease reported among all
ages, with the highest percentage in the teenage years [1]. It affects
10–20% of the entire population, hence causing AR to be the one
of the most chronic non-communicable disorder [2]. It is mostly
under diagnosed or even misdiagnosed, and mistreated, causing
harmful health related effects [3]. Allergic rhinitis is characterized
by inflammation in the nose as the immune system respond to
inhaled allergens in the air [4]. Signs and symptoms include a
runny or stuffy red and itchy nose, sneezing with watery eyes,
and swelling around the eyes [5]. Symptoms are rapidly emerging
with allergen exposure and associated with poor sleep hygiene
and work ability [6,7]. Mostly, allergic rhinitis is usually associated
with asthma, allergic conjunctivitis, or atopic dermatitis [8,9].
Septoplasty is the main surgical intervention for patients with
deviated nasal septum to relieve nasal obstruction [10-14]. In some
cases, additional turbinate surgery is performed. Most of studies
concerned with post-operative improvement reported that about
60% of patients undergoing septoplasty showed an improvement
in nasal breathing [15]. Septal perforation and septal hematoma
are recorded as complications along with decreased sense of
smell [16]. Temporary hypoesthesia of the front upper teeth after
surgery is not rare [17]. The post-operative complications intensity
or nature may be affected by whether the patients had allergic
rhinitis (AR) or not as AR may aggravates the nasal obstruction and
bleeding tendency [18]. The current study is aimed at revealing the
incidence of post septoplasty complications among both allergic
and non-allergic rhinitis patient groups.
Methodology
A retrospective Electronic record-based study was conducted
including all patients with clinically diagnosed nasal septum
deviation and underwent surgical intervention (Septoplasty) at
Khamis Mushait General Hospital during the period from January
2017 to end of May 2019. Apart from collecting Electronic data the
patients were also contacted via telephone to take verbal consent
to use their Electronic data and inquire about allergic symptoms
if already not mentioned in their record. Patients were excluded
if they had missing Electronic files, failure to give verbal consent
to participate (Telephonic), failure to contact the patient, or had
septoplasty as part of another procedure or along with another
surgery. After reviewing the medical files, the data was collected
on a pre-structured questionnaire. Data so collected included
patient’s demographics and post-operative complications for the surgery
such as nasal obstruction, nasal deformity, loss of smell
sensation, and others if any.
Data analysis
The collected data was coded, and statistical software IBM
SPSS version 22 was used to analyze it. The given graphs were
constructed using Microsoft excel software. All statistical analysis
was done using two tailed tests and alpha error of 0.05. P value
less than or equal to 0.05 was significant. Frequency in percent &
distribution of the different collected variables including patient’s
demographic data and post-operative complications were analyzed.
Crosstabulation was used to show the post-operative complications
distribution in relation patients’ history of having allergic rhinitis
using exact probability tests.
Results
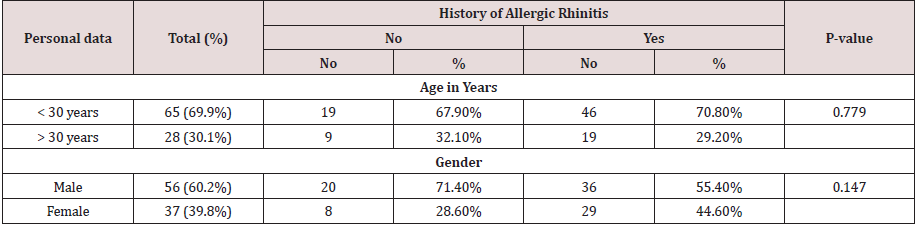
The study included a total sample of 93 patients out of 120
cases, sixty-five (69.9%) of the patients aged less than 30 years and
60.2% were males. Young aged persons constituted 70.8% of cases
with allergic rhinitis compared to 67.9% of cases without. Also,
females were 44.6% of cases with allergic rhinitis while 28.6%
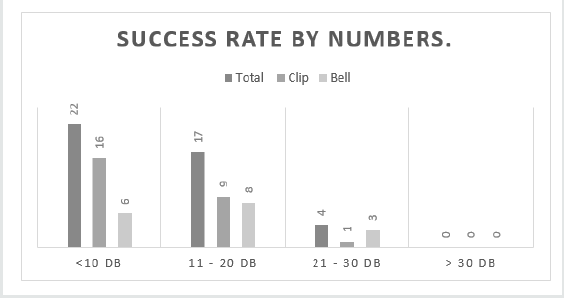
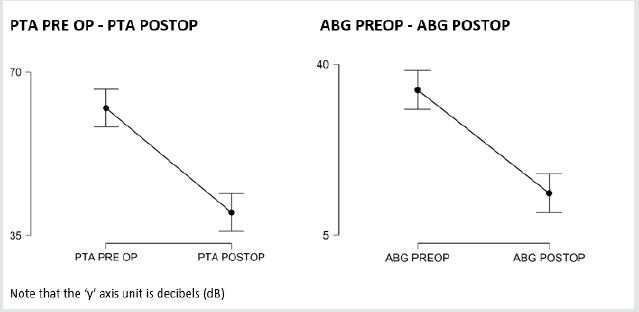
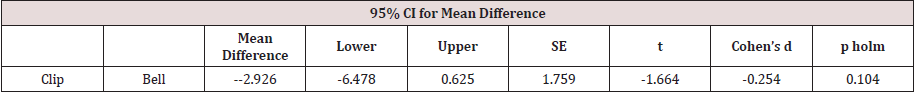
of those without allergic cases (Table 1). As for post-operative
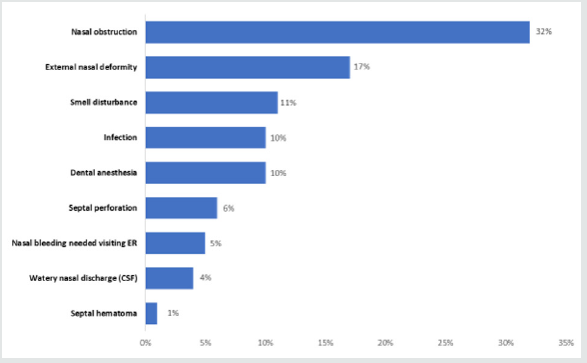
complications, figure 1 demonstrates that 32% of the cases had
nasal obstruction followed by external nasal deformity (17%),
smell disturbance (11%), dental anesthesia (10%), infection (10%),
septal perforation(6%),and nasal bleeding(5%). Considering
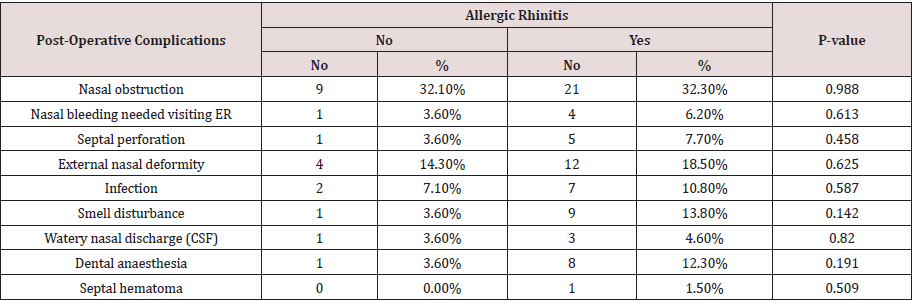
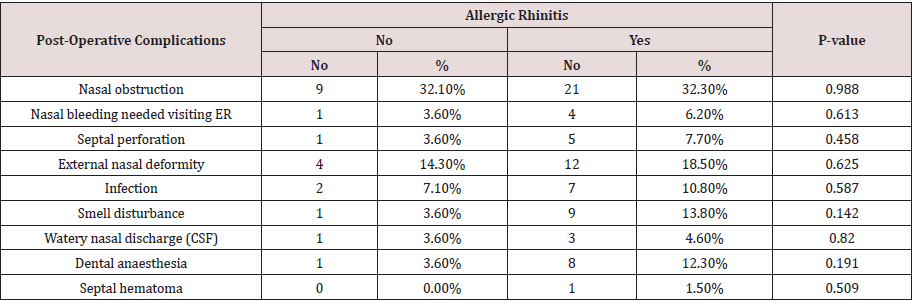
distribution of the complications according to the patients
with history of allergic rhinitis (Table 2), nasal obstruction was
diagnosed among 32.3% of the allergic patients compared to 32.1%
of cases with no allergic history (P=0.988). External nasal deformity
was recorded among 6.2% of the cases with AR compared to 3.6%
of others without AR (P=0.613) Septal perforation was recorded
among 7.7% of the cases with AR in comparison to 3.6% of the
cases without AR (P=0.458). Post-surgical infection with septal
abscess was diagnosed among 10.8% of the AR patients compared
to 7.1% of the other group (P=0.587). Regarding smell disturbance,
it was reported among 13.8% of the patients with AR compared
to 3.6% of those without AR (P=0.142). Watery nasal discharge
was diagnosed for 4.6% of the patients with AR in comparison
to 3.6% of those who were free of AR history (P=0.820). Dental
anaesthesia was complained by 12.3% of AR patients compared to
3.6% of others without AR (P=0.191). Lastly, Septal hematoma was
recorded one case with AR while was not recorded among any case
without history of AR (P=0.509) (Figure 1).
Figure 1: Post-operative complications among patients undergone septoplasty in Khamis Mushait general Hospital.
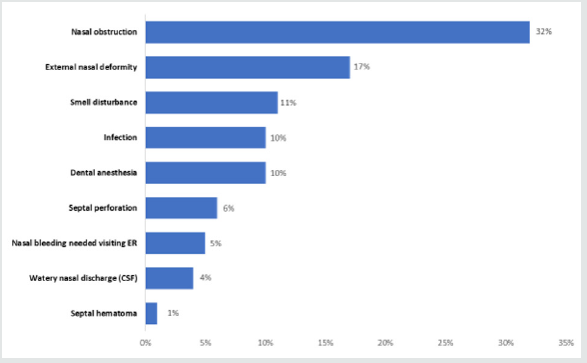
Table 1: Bio-demographic data of patients with nasal septum deviation in relation to history of allergic rhinitis in Khamis Mushait
general Hospital.
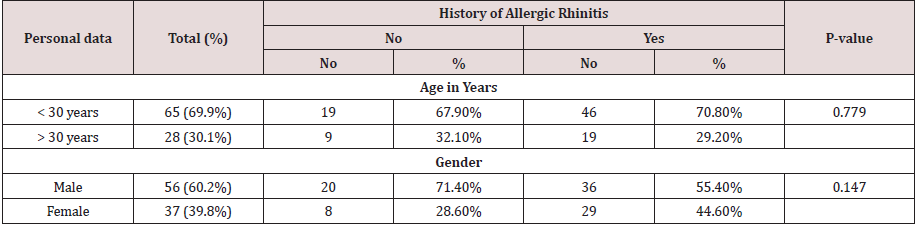
Table 2: Post-operative complications among patients undergone septoplasty according to history of allergic rhinitis, Khamis
Mushait general Hospital.
Discussion
High number of deviated nasal septum patients have
concurrent allergic rhinitis. Even though the conditions are not
similar, for patients with allergies or a deviated septum, there
are some similarities. For example, both diseases may lead to
sinus infection, both mimic the signs and symptoms of common
cold. Allergic rhinitis by the way of triggering allergic response
to airborne allergens while deviated septum can also have
nasal swelling and increased mucus, leading to same [19,20]. A
significant deviated nasal septum causes blockage on one side of
the nose and reduces airflow, causing difficulty breathing [21]. On
diagnosing nasal septum deviation, medical management using
topical nasal steroids, antihistamines, and decongestants as applied
for the nasal mucosa is typically attempted first. In case of failure,
a surgical intervention to correct the underlying septal deformity
is the second line [22-30]. The current study aims to clarify the
correlation between the allergic rhinitis and post septoplasty
complications as compared with non-allergic patients that will
reveal either significant or non- significant impact or difference.
The study revealed that nasal obstruction was the most reported
post septoplasty complication with close incidence in both allergic
rhinitis and non-allergic rhinitis groups [31,32]. This is against
what we expected that the postoperative nasal obstruction will be
higher in AR patients as a result from AR itself. this observation is
supported by another study which was done in our region (South
of Saudi Arabia) and found positive outcome of septoplasty for
those AR patients with nasal obstruction postoperatively [33]. The
second most common postoperative complication is external nasal
deformity in both groups, slightly higher among AR patients’ group.
The least complication is similar in both groups which is septal
hematoma. The other postoperative complications are ordered
from more to less common among the patients with AR as following,
smell disturbance, dental anaesthesia, infection, perforation,
nasal bleeding then watery discharge. While among the patients
without AR are infection, nasal bleeding, smell disturbance, dental
anaesthesia, perforation then watery discharge which are having
the same incidence rate. All post septoplasty surgical complications
that were recorded higher among allergic rhinitis cases except nasal
obstruction but the higher rate among AR cases was insignificantly
different than other for the sample in total.
Conclusion
In conclusion, the study revealed that postoperative nasal
obstruction complication is the most one with similar incidence rate
in both allergic and non-allergic rhinitis patient groups while the
least one is septal hematoma. The other postoperative complications
are different in both groups regarding the commonness. All post
septoplasty complications except nasal obstruction are slightly
higher among allergic rhinitis cases. Our study opens more query
and understanding to the pathophysiology of allergic rhinitis and
its impact on the post-surgical outcomes.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/