Lupine Publishers | Journal of Otolaryngology
Statement of The Problem
This provides an overview of Allergic Rhinitis and its management. It
is very useful for students of Rhinology and clinicians
managing this disease. It introduces them to a systematic approach of
assessing allergic rhinitis patients which is very commonly
found in most populations and causes considerably morbidity. Allergy per
se is a very difficult subject to master and it is with great
perseverance one can treat patients suffering from this condition. The
cornerstone of managing a patient of allergic rhinitis is first
and foremost obtaining a good history. This is to be followed by a
thorough examination and investigations. The general practitioner
is the first expert to be involved in management of allergic rhinitis
patient followed by specialists otorhinolaryngologists, and finally
by allied healthcare personnel. Inflammation of nose and paranasal
sinuses are characterized by two or more symptoms-namely,
either nasal blockage; obstruction; congestion or nasal discharge.
Associated symptoms include facial pain; pressure and either
reduction or loss of smell. Certain diagnostic endoscopic signs of nasal
polyps and or mucopurulent discharge and or mucosal
oedema in the middle meatus and or CT changes of mucosa within the
ostoemeatal complex, and or sinuses are seen. Definitions,
aetiologies, clinical presentations, diagnosis; prognosis and management
of allergic rhinitis is dealt with. Common allergens causing
the disease are mentioned, pathophysiology and classification of
allergic rhinitis is discussed in detail. Different types of allergen
testing are highlighted along with their specific role and uniqueness.
Principles of immunotherapy in treatment of allergic rhinitis
are discussed here. Health effects of allergic rhinitis along with its
impact on physical quality of life is mentioned. The basic idea
of this presentation is to improve diagnostic accuracy by promoting
appropriate use of ancillary tests like nasoendoscopy, allergy
testing, computed tomography etc. and reduce inappropriate antibiotic
use. The basic treatment plan of allergic rhinitis is according
to the severity and duration. It consists of allergen avoidance,
pharmacotherapy, allergen immunotherapy and surgery which has
limited role.
Keywords: Allergy; Rhinitis; Pollens; Molds; Insects; Penicillium; Cladosporium; Hypersensitivity; Histamine; Hay fever; Rose
Fever; Transverse Nasal Crease; Rhinorrhea; Allergic Salute; Allergic Shiners (Dennie -Morgan Lines); Cobblestone Appearance
Of Oropharynx; Scratch Test ; Intradermal Test; Patch Test; Rhinomanometry; Antihistaminics; Immunotherapy; Topical Nasal
Steroids; Cochrane; Mast Cell Stabilizer
Abbreviations: IgA: Immunoglobulin A, IgE: Immunoglobulin E, AR: Allergic Rhinitis; NAR: Non-Allergic Rhinitis; ARIA:
Allergic Rhinitis & its Impact on Asthma; Greater than; Less than; TM: Tympanic membrane; NPT: Nasal Provocation Test; n NO:
Nitrogen in Nitric Oxide; PNS: Para Nasal Sinuses; OM: Occipito Mental; CECT: Contrast Enhanced Computerized Scan; L.A: Local
Anaesthesia GA: General Anaesthesia; PQLI: Physical Quality of Life Index; WAO: World Allergy Organization; SCIT: Subcutaneous
immunotherapy; SLIT: Sublingual immunotherapy; AIT: Allergic Immunotherapy; e-Health: Electronic Health; DBPC: Double Blind
Placebo Controlled; RCT: Randomized Controlled Trial; FDA: Food & Drug Administration federal agency in USA; SMD: Submucous
Diathermy; IT: Inferior turbinate; FESS: Functional Endoscopic Sinus Surgery; OMC: Osteo Meatal Complex
Introduction
Rhinitis is a common presentation in E.N.T. clinics across the
globe & allergy compounded with it causes even more difficult to
treat for the clinician. This article is useful and handy for students
and clinicians managing Allergy& Rhinitis. There is something in
this for everyone-General Practitioners, Otorhinolaryngologists,
Allergologists, Rhinologists and Allied Healthcare personnel.
Special computer based newer modalities of investigations are
highlighted in this which helps in assessing the nasal function of the
affected patient. It’s very common to sometimes feel like sneezing
& have running nose but please see a doctor if the feeling persists
and do take care of yourself. Allergic Rhinitis is made so easy to
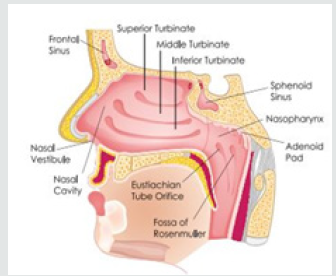
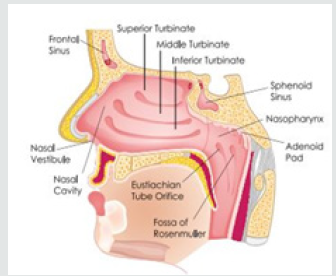
comprehend. Nasal function includes temperature regulation,
olfaction, humidification, filtration and protection [1]. Nasal
lining contains secretion of IgA, proteins and enzymes. Nasal cilia
propel the matter towards the natural ostia at frequency of 10-15
beats; min. Mucous moves at a rate of 2.5 -7.5ml. per min (Figure
1). Rhinitis is the presentation of two or more nasal symptoms
for more than one a day namely Nasal congestion; obstruction,
Rhinorrhea, Sneezing, Itching, Impairment of smell. Rhinitis occurs
most commonly as Allergic Rhinitis. Non-infectious rhinitis has
been classified as either Allergic or Non-Allergic Rhinitis. Allergic
Rhinitis affects 15-30% of population with a wide geographic
variance. It is more common in children & adolescents. 50% of
all rhinitis in E.N.T. Clinics is Allergic Rhinitis. Allergic Rhinitis is
defined as immunologic nasal response, primarily mediated by IgE.
Non-Allergic Rhinitis is defined as rhinitis symptoms in the absence
of identifiable allergy, structural abnormality or sinus disease. So,
Allergic Rhinitis is an inflammation of the nasal mucosa, caused by
allergen. It is the most common Atopic allergic reaction.
Figure 1: The Human Normal Eye Anatomy.
Aetiology
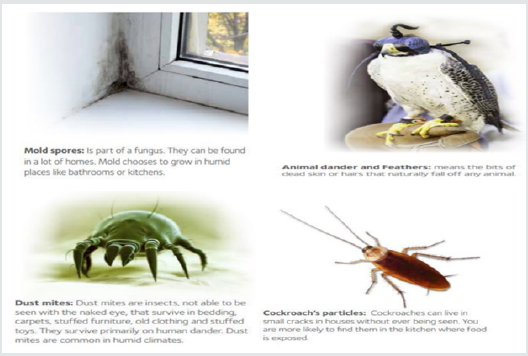
Aetiology is classified as Precipitating factors and Predisposing
factors. Precipitating factors are classified into aerobiological flora
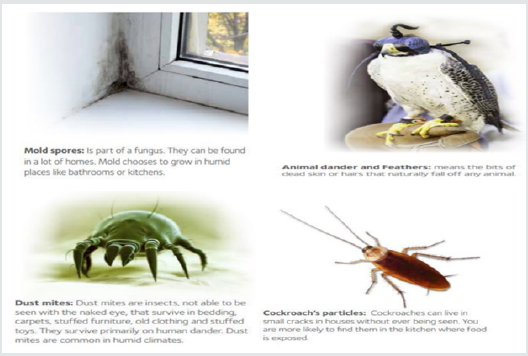
and nasal physiology. Aerobiological flora are Allergens present
in the environment, House dust & dust mites, Feathers, Tobacco
smoke, Industrial Chemicals and Animal dander. Nasal physiology
are Disturbances in normal nasal cycle. Predisposing factors are
classified into genetic, endocrine, psychological, focal sensitivity
tests, infections, physical, age & sex, IgA deficiency and common
allergens [2]. Genetic factors indicate towards Multiple gene
interactions are responsible for allergic phenotype. Chromosomes
5,6,11,12 & 14 control inflammatory process in atopy. 50% of AR
pts. Have positive family history. Endocrine factors are Puberty,
Pregnancy; Postpartum stages and Menopause. Infections such as
Fungal. Physical factors are Degree of pollution of air, Humidity &
Temperature differences, Temperature changes. Common allergens
such as pollens (Spring tree pollens (Maple ; Alder ; Birch), Summer
grass pollen (Blue grass, Sheep sorrel etc.), Autumn Weed pollen
(Ragweed)), molds) Penicillium, Cladosporium etc.), INSECTS
(Cockroaches, Houseflies, Fleas, Bedbugs) (Figure 2). Rhinitis is the
presentation of two or more nasal symptoms for more than one a
day namely Nasal congestion; obstruction, Rhinorrhea, Sneezing,
Itching, Impairment of smell. Rhinitis occurs most commonly as
Allergic Rhinitis. Non-infectious rhinitis has been classified as either
Allergic or Non-Allergic Rhinitis. Allergic Rhinitis affects 15-30% of
population with a wide geographic variance. It is more common
in children & adolescents. 50% of all rhinitis in E.N.T. Clinics is
Allergic Rhinitis [3]. Allergic Rhinitis is defined as immunologic
nasal response, primarily mediated by IgE. Non-Allergic Rhinitis is
defined as rhinitis symptoms in the absence of identifiable allergy,
structural abnormality or sinus disease. So, Allergic Rhinitis is an
inflammation of the nasal mucosa, caused by allergen. It is the most
common Atopic allergic reaction.
Figure 2:
Pathophysiology
Immunoglobulin IgE mediated type 1 hypersensitivity response
to an antigen (allergen) in a genetically susceptible person. IgE
is produced from plasma cells & the process is regulated by
T-Suppressor lymphocytes or T-helper cells. IgE has affinity for mast
cells & basophils and gets fixed to the surface of mast cells by its Fc
end. Type 1 Hypersensitivity causes local vasodilation & increased
capillary permeability. There is edema of the submucosal tissue
by allergic fluid followed by infiltration by eosinophils and plasma
cells leading to vascular dilatation which causes engorgement
of the inferior turbinates and there is increased activity of seromucinous
glands [4]. Histamine exerts its pharmacologic effect on
smooth muscle, vascular endothelium & mucous glands. Number of
IgE molecules has been estimated as 5300 to 27,000 in non-allergic
subject & 15,000 to 41,000 in allergic subjects. Hypersensitivity of
the host depends on antigen dose, frequency of exposure, genetic
make-up, and hormone activity of the body.
Classification
Allergic Rhinitis is currently classified into intermittent and
persistent. In intermittent AR the symptoms are present less than
4 days per week and less than 4 weeks per year [5]. In persistent
AR the symptoms are present for greater than 4 days per week and
for greater than 4 weeks per year. The severity of AR is classified
into mild and moderate to severe. Mild AR doesn’t interfere with
daily activities or doesn’t produce any troublesome symptoms.
Moderate to severe AR interferes at least with one of the factors
such as impaired sleep, hampered daily activities/work, school/
sick absenteeism, also produces troublesome symptoms. AR
is formerly classified into seasonal and perennial based on the
allergens. Seasonal Hay Fever, misnomer- no hay/no fever. Summer
Cold caused by viruses causing URTI. Rose Fever seen usually in
Indian Subcontinent (colorful/fragrant flowering plants). Perennial
Allergens present throughout the year.
Signs and symptoms of AR
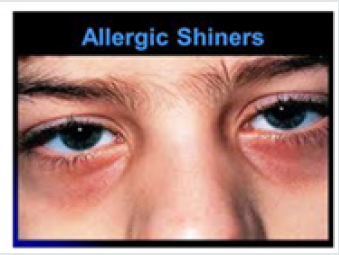
Symptoms of AR are sneezing, itching of eyes, ears & palate,
rhinorrhea, postnasal drip, congestion, anosmia, headache, otalgia,
epiphora, red eyes, swollen eyes, fatigue, drowsiness and malaise.
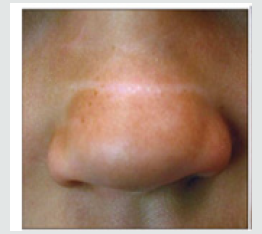
Figure 3(a): Transverse Nasal Crease
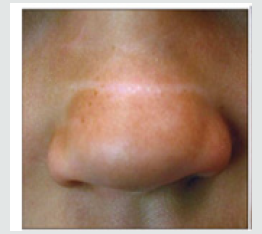
Figure 3(b): Allergic salute

Figure 3(c): Allergic shiners (Dennie-Morgan lines).
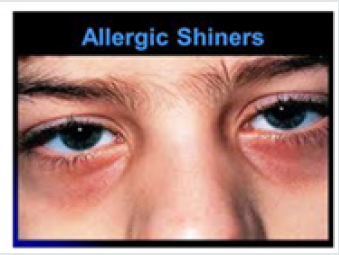
Figure 3(b): Cobblestone appearance of oropharynx.

Physical Examination: During Physical examination we check
for TRANSVERSE NASAL CREASE (Horizontal crease across the
lower half of the bridge of nose), RHINORRHOEA (Thin watery
secretions from nose) (Figure 3). Associated features with AR are
Injected & swelling of palpebral conjunctiva with excess tearing,
Retracted T.M.’s, Overbite, Periorbital oedema.
Investigations
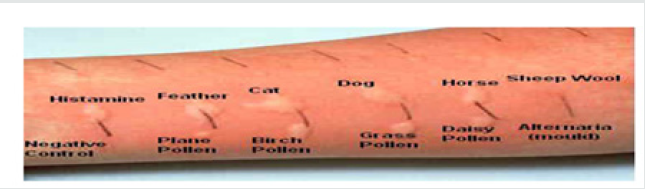
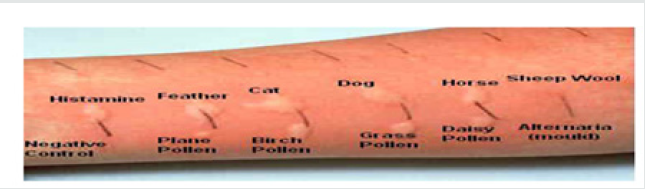
Skin prick tests---gold standard. This is also known as Scratch
Test; Intradermal Test. Controlled amounts of allergen & control
substances are introduced into the skin this procedure is convenient,
safe & widely accepted (Figure 4). Goal of the investigation is the
detection of immediate allergic response caused by release of mast
cells or basophil IgE specific mediators Wheal; Flare after 15 mins
[6]. More investigations are such as RAST-Radio-Allergo-Sorbent
Test for specific IgE estimation. PRIST-Plasma Reactive Immuno-
Sorbent Test for specific IgE estimation. SET Test-Skin End-Point
Titration Test Latest skin test for allergy & is more reliable. Less
common tests are total serum IgE, total blood eosinophil count,
nasal smears may show increased eosinophilic level, PATCH TEST
is used to determine delayed type hypersensitivity & the allergen
is placed in the skin for 48hrs [7]. The area of reaction is noted and
if any allergens present are identified. This is more useful in skin
problems & food allergy.
Figure 4:
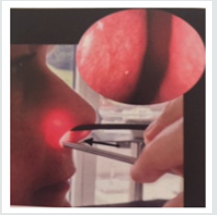
a) Nasal provocation tests (NPT)
Figure 5(a): Rhino meter.

Figure 5(b): Spraying Device for NPT.
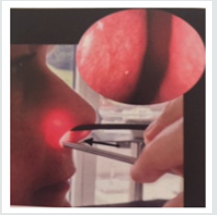
The potential allergen is sprayed into the nose & the number of
SNEEZES counted or any change in Rhinomanometry is noted. Very
time-consuming test as each allergen takes 20 mins. To test in order
to allow the nose to return to normal after the challenge. It is useful
for rare & occupational allergens. Contraindications of NPT are
Pregnancy; < 5yrs. age; Recent nasal surgery <8 wks; Uncontrolled
asthma, Nasal; systemic corticosteroids should be avoided for 1wk
& Antihistaminics for 72hrs (Figure 5).
New Diagnostic Methods
Exhaled Nitric Oxide (E No): Like e NO in asthma, n NO is a noninvasive
marker. Potentially suitable to monitor upper airway
inflammation following allergen-induced late response. In AR
pts., increased levels of n NO have been measured. However, the
applicability of n NO as a marker of upper airway inflammation
awaits validation. Exhaled nitric oxide (e NO) is currently the
MOST RELIABLE MARKER of rhino-bronchial inflammation, but its
routine assessment is difficult as the test is available only in highly
specialized centers.
Other Investigations
X-RAY PNS-Water’s (OM view). CECT of PNS…2mm. Coronal
cuts are preferred. NASOENDOSCOPY. under L.A.; G.A. Hopkins rod
0º; 30º; 70º). Evaluate the individual for asthma. At some centres
FAST-Fluro Allergo Sorbent Test is done.
Complications of AR
Complications of AR are allergic asthma, chronic otitis media,
hearing loss, chronic nasal obstruction, sinusitis, orthodontic
malocclusion in children (Figure 6).
Figure 6: The Human Normal Eye Anatomy.

Prognosis
Treatment is available & pts. remain asymptomatic only until
re-exposure to allergic antigen. There is no evidence of mortality
from the disease but there is very high morbidity. PQLI is affected.
Seasonal allergic symptoms improve as patients age.
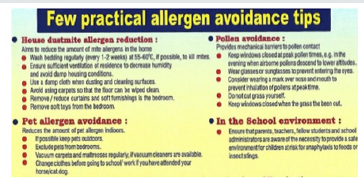
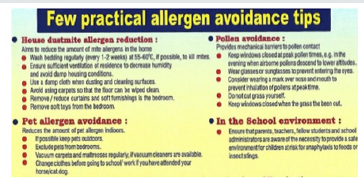
Management of AR
Management of Allergic Rhinitis includes Allergen avoidance
& environmental control measures, Medical; pharmacologic
treatment, Immunotherapy and Surgery [8]. Choice of treatment
will depend on efficacy, safety, cost-effectiveness, patient
preferences, combination, objectives of treatment, likely adherence
to recommendations, severity & control of disease and presence of
co-morbidities. Practical allergen avoidance tips given by WAO for
public education purposes are as follows in (Figure 7).
Figure 7: The Human Normal Eye Anatomy.
Pharmacotherapy
Oral antihistaminic are
1ST GEN: - Chlorpheniramine maleate; Diphenhydramine;
Clementine.
2ND GEN: - Loratadine; Terfenadine; Acrivastine
3rd GEN.: - Fexofenadine; Cetrizine. Topical application of
Azelastine.
NEWER - Desloratadine; Levocetrizine.
Acute Phase Medications
Antihistaminics are effective in blocking histaminic effects.
(Runny nose; Watery eyes). Side Effects of antihistaminics
are Sedation, Dry mouth, Nausea, Dizziness, Blurred vision,
Nervousness. Non-sedating antihistaminics (Cetirizine;
Loratadine) has fewer side effects. Fexofenadine is more effective
(has a lower risk of cardiac arrythmias). Decongestants will Shrink
mucous membranes by vasoconstriction. These are available OTC;
in combination with antihistaminic, analgesics & anti cholinergic
[9]. Anticholinergic Agents Inhibit mucous secretions which acts
as drying agents. Topical Eye Preparations reduces inflammation;
relieves burning and itching (Figure 8).
Figure 8:
Preventive Therapy
Intranasal Corticosteroids Reduces inflammation of mucosa,
prevents mediator release, can be used safely daily, can be
given systemically as a short course during a disabling attack.
Intranasal Cromolyn Sodium Mast cell stabilizer Prevents release
of chemical mediators. Oral Mast Cell Stabilizer, Ophthalmic
solution cromolyn. Topical nasal steroids are dexamethasone,
beclomethasone dipropionate, triamcinolone acetonide, flunisolide,
budesonide, fluticasone propionate, mometasone furoate and
ciclesonide [10]. LEUKOTRIENE RECEPTOR ANTAGONISTS
(ANTI LEUKOTRIENE AGENTS) are MONTELEUKAST(Singular);
ZAFIRLEUKAST(Accolate) & PRANLEUKAST. These drugs reduce
inflammation, oedema & mucous secretions of Allergic Rhinitis.
ZILEUTON (5-Lipoxygenase inhibitor) is a similar drug & is used in
many parts of the world.
Immunotherapy (AIT)
SCIT is effective in seasonal pollinosis & mite allergy. SLIT is
Effective & safe alternative, best in seasonal AR. COCHRANE reviews
shows that both are equally effective & the patient is in equipoise.
These are more effective in adult pts. 3yrs. Of treatment with both
SCIT & SLIT has been shown to provide long term clinical benefits
for at least 2 yrs. after their discontinuation. The choice of therapy
depends on grounds of convenience, availability of resources &
personal preferences. SCIT requires administration in a specialist
clinic whereas SLIT can be self-administered.
Current Concepts & Future Needs
Although AIT is considered a safe & effective treatment for
AR, however, its clinical effect is still contested by many due
to: Heterogenicity in clinical trial designs, Study populations,
Therapeutic formulations, Efficacy criteria. There is ample scope
for physicians, patient organizations, companies & regulators to
improve clinical trials in AIT and, to provide patients with better
treatments. Inclusion of allergic pts. with relevant diseases(s) in
AIT trials. Exclusion of polyallergic pts. (with clinically relevant,
overlapping allergen exposures) in AIT trials. Clinically defined
responders in AIT trials. Allergen exposure chambers in AIT trials.
Differences in regional & seasonal exposures. Adaptive trial designs
should be discussed with regulatory bodies. Patient-to-patient
differences in treatment adherence & allergen exposure. (Use
of “e-health” is recommended). The placebo effect in AIT is to be
considered. Ethical & technical aspects of DBPC; RCT’s, especially in
paediatric populations. The importance of safety reporting. (WAO
guidelines for reporting systemic & local adverse events should be
applied).
Omalizumab for Treatment of AR
Figure 9:

(Figure 9) This is a new treatment strategy for allergic rhinitis
DBPC study of RAGWEED immunotherapy7 is done. Prohibitive
high cost. It is not FDA approved for this indication. Periodic use
is justified in treatment of resistant patients especially those with
seasonal disease. This drug acts by removal of circulating free IgE
by the recombinant humanized monoclonal anti IgE antibody.
Surgical Treatment: Surgical treatment has limited use, SMD of
I.T. reduces the size of boggy turbinates. Septoplasty is done for
the Correction of septal deviation. FESS is done for the Clearance
of sinuses and OMC If indicated. VIDIAN Neurectomy is done in
certain selected cases.
Surprising Relief for Stuffy Nose: Sex: According to Dr. Michael
Benninger, Otolaryngologist, Chairman of Cleveland Clinic’s Head
& Neck Institute, in a study done in May 2018 has some surprising
findings. The potential effect of sexual activity works the same
for man & women. Swollen tissues in nose block the passages in
AR creating congestion & making it harder to breathe. During
arousal, the Sympathetic NS gets into play, adrenaline levels go
up & blood vessels constrict. Less blood flow to the nose means
less inflammation, so the nose opens up & one can breathe more
easily. Lying on back position for both men and women, one cannot
experience the same level of congestion relief due to effects of
gravity.
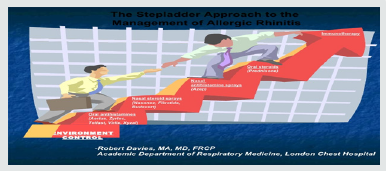
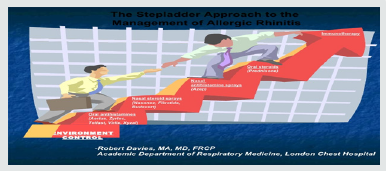
Stepladder Approach in Treatment of AR: (Figure 10) Allergic
Rhinitis Guide: Frequently Asked Questions (FAQ’S)
Figure 10:
a) What is common medication mistake that people make?
b) How long should one stay on allergy treatment?
c) How can one differentiate between common cold & AR?
d) What are the side effects of allergy medications?
e) How to use nasal sprays? (Figure 11)
Figure 11:

f) Are the steroids in nasal sprays safe?
g) What is the difference between the nasal medications & oral
medications?
h) How quickly can one expect to get relief from allergy treatment?
i) Taking corticosteroids inhalers to control asthma symptoms,
can one also take allergy medications?
j) What are the types of allergy tests? IgE skin test; Intradermal
test; Specific IgE in blood.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/