Lupine Publishers | Journal of Otolaryngology
Background: The human voice is one of the most important tools in human every day. Communication and voice were probably
important to human communication even before language evolved. Voice Quality can be affected in patients with thyroid disease
like, loss of vocal range, low speaking fundamental frequency (especially in women), coarse and gravelly vocal symptoms, weak
voice, and breathy quality, reduced Intensity and changes of the singing voice.
Purpose: The aim of this work is to identify auditory perceptual voice changes and Severity in patients with thyroid and/or
parathyroid disease preoperatively.
Methods: 60 adult subjects their age ranged between 20 and 60 years old, both males and females, divided into two groups
were included (Group A): 30 patients diagnosed with thyroid and/or parathyroid Disease preoperatively. (Group B): 30 healthy
normal subjects. Both groups were undergone to Modified GRBAS scale, Voice Recording, and Flexible nasofibrolaryngoscopy.
Results: There is difference between the two groups regarding the presence or absence of dysphonia, chewing and swallowing,
and parameters of APA (auditory perceptual assessment) except register.
Conclusion: The perceptual measure of voice by modified GRBAS,
revealed significant differences in (overall grade of dysphonia,
pitch, and loudness, of voice) between the individuals with thyroid
disease and those in an age and gender-matched control group.
If surgeons can screen for pre-surgical dysphonia, the rate of
indeterminate postsurgical dysphonia may be reduced, or at least
explained and prepared for.
Keywords: Voice parameters; thyroid diseases; pre-operative assessment
Introduction
The human voice is one of the most important tools in human
everyday communication and the voice was probably important
to human communication even before language evolved. Also,
long before the infant develops language; it expresses important
information by means of its voice organ [1]. Voice Quality can be
affected in patients with thyroid disease. There are number of voice
problems occur in thyroid disease including loss of vocal range, low
speaking fundamental frequency (especially in women), coarse
and gravelly vocal symptoms, weak voice, breathy quality, reduced.
Intensity and changes of the singing voice [2]. Vocal impairment in
thyroid disease may be related to structural or `functional changes
in the larynx or as the thyroid gland is closely related to the larynx
via both innervation and blood supply. However, the nerves and
arteries of the thyroid and larynx are intertwined, thus damage to
one structure could easily affect the other structure [3]. Thyroid
disease may or may not have a noticeable impact on laryngeal functioning. If a patient develops massive tumor, compression of
the vocal folds results in dysphonia, stridor and dyspnea. When
cervical nodes metastasize, vocal fold paralysis can occur related
diseases that often co-occur with nodules such as hypothyroidism
and hyperthyroidism may impact the laryngeal mechanism [3].
Voice related outcomes were reported post-operatively in patients
who received thyroid surgery.
Patients were tested prior to surgery and postoperatively with
the Visipitch oscilloscope, an objective tool used for voice analysis,
which measures pitch and amplitude over time. Patients were also
given a questionnaire following surgery. Patients were considered
to be “worse” if there was a decrease in maximum phonation time
more than 2 seconds, an increase in perturbation greater than
.05%, or a decrease in percentage voiced by 2%. “Improvement”
was judged by using the same guidelines in the opposite direction
[4]. Patients may have voicing abnormalities before thyroid surgery
is performed and surgery may improve or worsen the voice
irrespective of the pre-operative voice status [4]. There is lack
of information on the incidence of voice disorders in those with
thyroid disease [5] reports the possibility of dysphonia, stridor and
dyspnea in those with thyroid tumors. Hypothyroidism can cause
perceived voice changes such as lower pitch, roughness, decreased
range, and vocal fatigue; whereas hyperthyroidism can cause
shaky voice, breathy vocal quality, and reduced intensity beside
that the impact of aging on the larynx can also cause perceptual
changes in the voice [3]. Modified GRBAS has been shown to be a
reliable measure for identifying perceived vocal changes. The ease
of use and high predictive value of this measure makes it ideal
for measuring voice parameters as experienced by the listener
[5]. If those with thyroid disease often display vocal dysfunction,
detection of these symptoms could aid in early detection of thyroid
disease. Further, obtaining a baseline for voice dysfunction in those
with thyroid disease could facilitate documentation of the recovery
process. Moreover, baseline data could help surgeons determine
the success of their surgical techniques based on postoperative
vocal function [6].
Objectives
The aim of this work is to identify auditory perceptual voice
changes and Severity in patients with thyroid and/or parathyroid
disease preoperatively.
Subjects & Methods
This study included 60 adult subjects divided into two groups:
a) Group A: 30 patients diagnosed with thyroid and/or
parathyroid Disease preoperatively
b) Group B: 30 healthy normal subjects their age ranged
between 20 and 60 years old, both males and females. Both
groups were matched in age and gender.
Exclusion criteria: Applied on both groups
a) Smoking, alcohol or drug abuse.
b) Those on any regular medication which might have an
effect on voice quality.
c) Those with respiratory tract infection on the day of
assessments.
d) History of severe respiratory allergies, asthma,
neuromotor impairment, hearing impairment, or psychiatric
problems.
e) History of neck surgery in the past years.
f) History of misuse and abuse of voice.
g) Gross laryngeal lesions by laryngoscopy.
All patients were subjected to:
1) Protocol of voice assessment that was applied in
phoniatrics unit Beni-Suef university hospital and in Alexandria
University hospital.
2) Auditory perceptual assessment (APA) GRBAS
modification: [7] described a modified scale for Evaluation of
dysphonic voice which called a “modified GRBAS scale” where
the followings were evaluated:
a) Overall grade: Normal (0), Slight (1), Moderate (2) or
Severe (3).
b) Character (quality):
i. Strained (S): perception of excessive vocal effort.
ii. Leaky (L): excessive air escape during phonation under
pressure.
iii. Breathy (B): excessive air escape during phonation not
under pressure.
iv. Irregular or “rough” (I): lack of clear vocal quality.
c) Pitch: Overall increase, Overall decrease, Diplophonia
d) Register: Habitual, Modal or falsetto; Tendency to vocal
fry at the end of phrase; Register break
e) Loudness: Excessively loud, Excessively soft, Fluctuating
f) Glottal attack: Normal, Soft, Hard
g) Associated Laryngeal Functions: Cough, Whisper, Laugher
Voice recording was carried out in a sound treated room, the
patient was sitting 10 cm away from the microphone and Off-axis
positioning (45–90 from the mouth axis) reduces aerodynamic
noise from the mouth during speech. Regarding voice/speech
material, examples of protocol for standard recording were as
follows:
a. The patient counted to ten at comfortable pitch and
loudness.
b. /a/: at (spontaneous) comfortable pitch/loudness,
recorded three times to evaluate variability of quality.
c. /a/: slightly louder to evaluate the possible change in
quality (plasticity)
d. A single sentence or a short standard passage Phonetic
selection can be useful, such as a short sentence with constant voicing (no voiceless sounds and spoken without interruption)
and no fricatives.
3) Indirect laryngoscope examination: The larynx was
visualized simply by using laryngeal mirror. For assessment of
vocal fold structure, configuration and gross mobility.
4) Flexible nasofibrolaryngoscopy: To visualize the vocal
folds during various articulatory maneuvers and allows
visualization not only the larynx but also of supra glottal
structure and even velopharyngeal mechanism [8].
Statistical tests used in this thesis were:
a. Description of qualitative variables by frequency and
percentage.
b. Description of quantitative variables in the form of mean
and standard Deviation (mean ± SD).
c. Chi-square (x2) test was used for comparison of
qualitative variables with each other.
a) Comparison between quantitative variables was carried
by using: -Student t-test of two independent samples.
Significance level (p) was expressed as following:
a. P value > 0.05 is insignificant (NS).
b. P value < 0.05 is significant(S).
c. P value < 0.001 is highly significant (HS).
Results
The study’s sample included 60 subjects their ages ranged
between (22 and 58 years) with a mean (36.5±8.6) table (2), they
were 8 males and 52 females and were divided into two groups
(Group A): 30 patients diagnosed with thyroid and/or parathyroid
disease preoperatively consisted of 4 males and 26 females their
ages ranged between (23 and 58 years) with a mean ± SD (36.8±8.5).
(Group B): 30 healthy normal subjects consisted of 4 males and 26
females their ages ranged between (22 and 57 years) with a mean ±
SD (36.2±8.7). Both groups were matched as regard age and gender.
Results of Auditory Perceptual Assessment (APA) by
GRBAS modification
Figures 1-10.
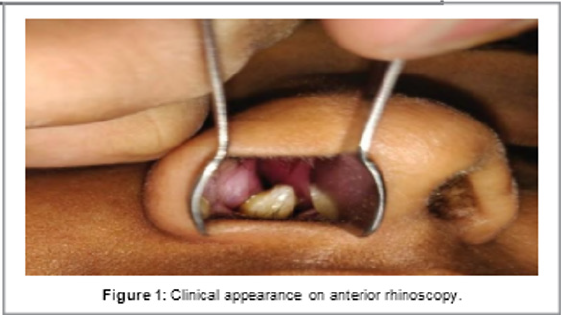
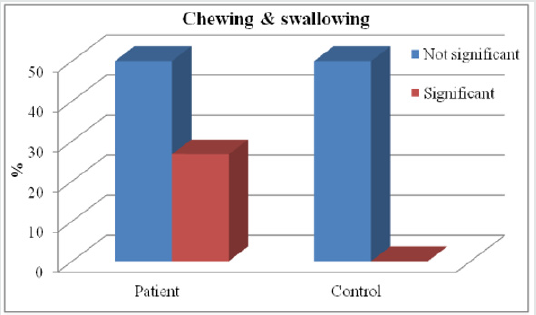
Figure 1: Shows highly significant difference between the two groups (A&B) regarding chewing and swallowing affection.
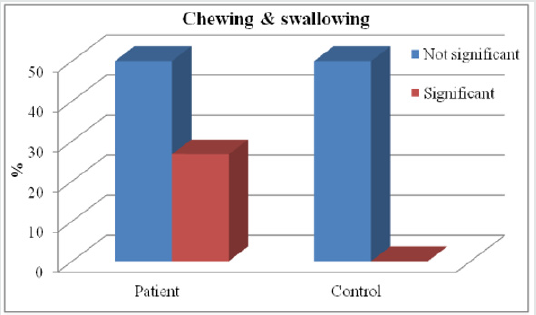
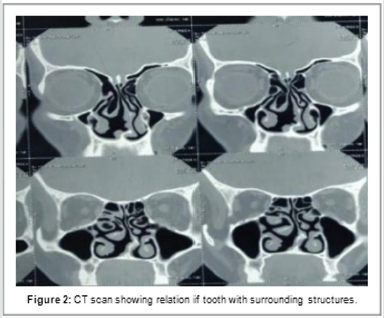
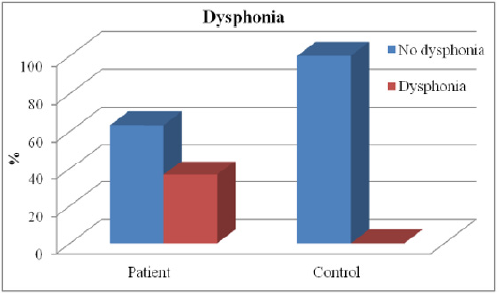
Figure 2: Shows highly significant difference between the two groups (A&B) regarding dysphonia.
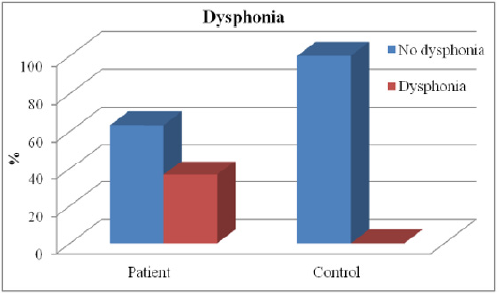
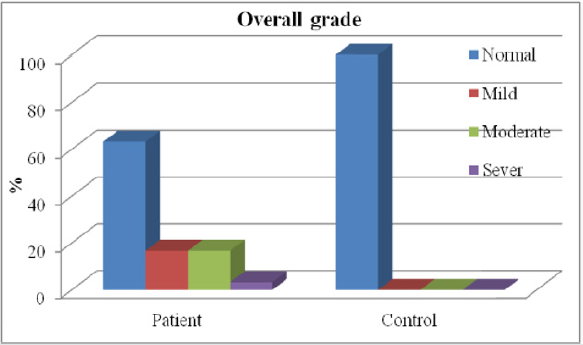
Figure 3: Shows highly significant difference between the two groups (A&B) regarding overall grade.
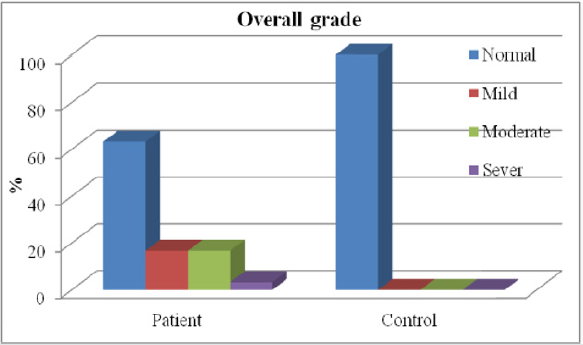
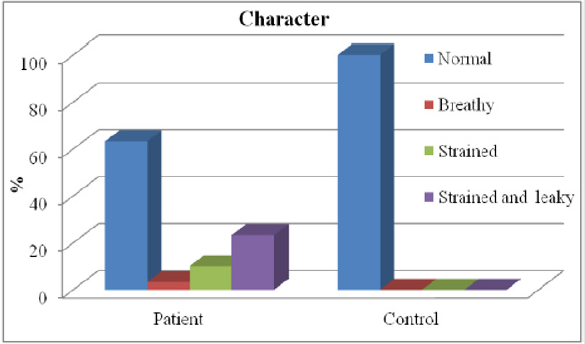
Figure 4: Shows highly significant difference between the two groups (A&B) regarding character.
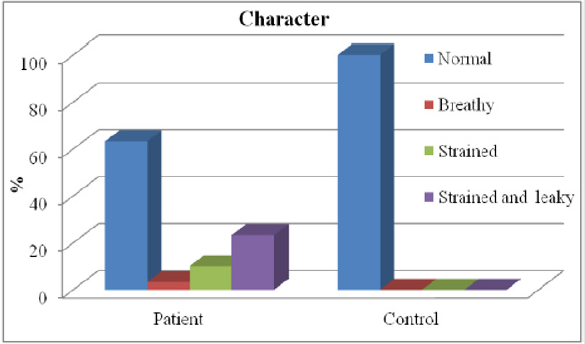
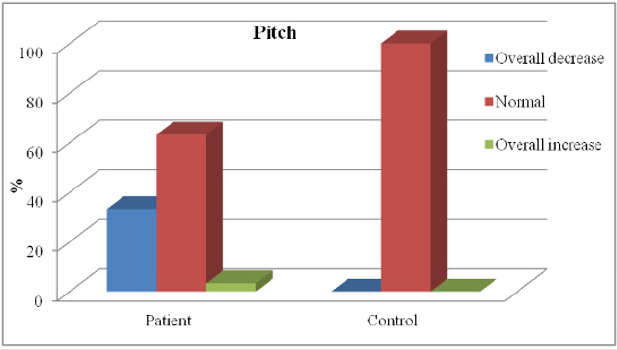
Figure 5: Shows highly significant difference between the two groups (A&B) regarding pitch.
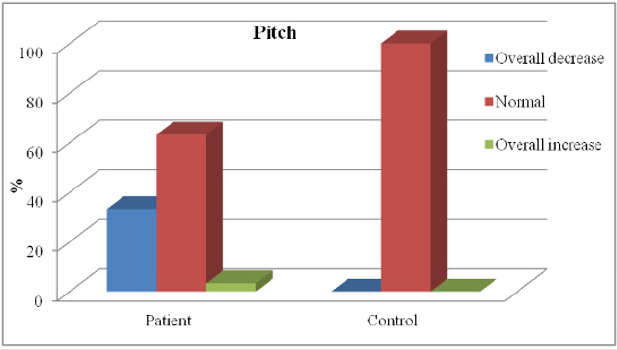
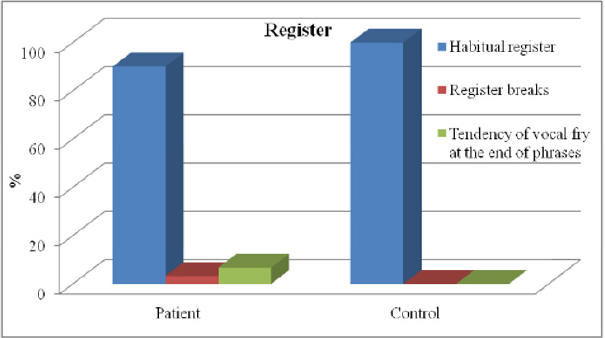
Figure 6: Shows no significant difference between the two groups (A&B) regarding register.
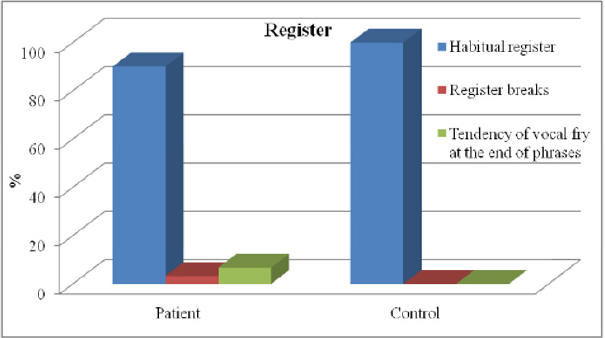
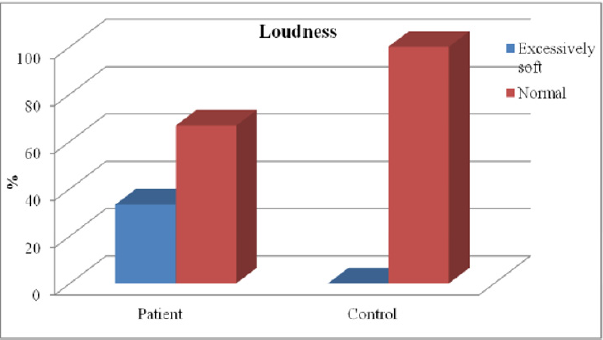
Figure 7: Shows highly significant difference between the two groups (A&B) regarding loudness.
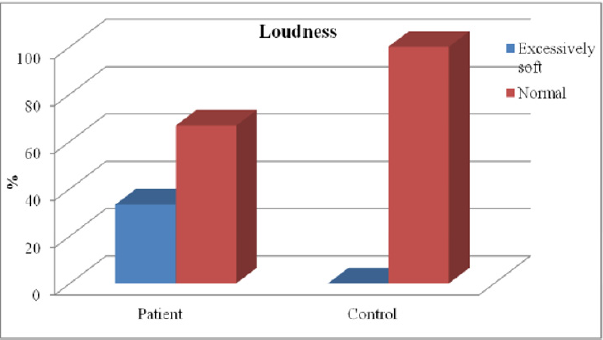
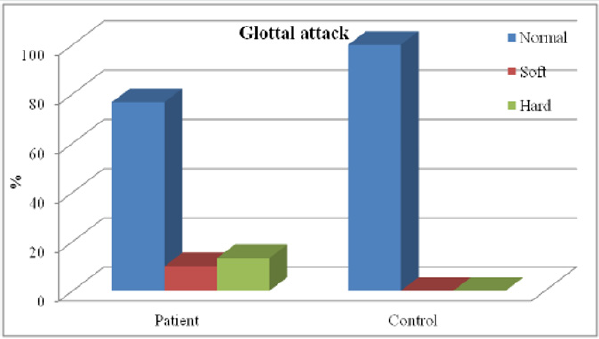
Figure 8: Shows significant difference between the two groups (A&B) regarding glottal attack.
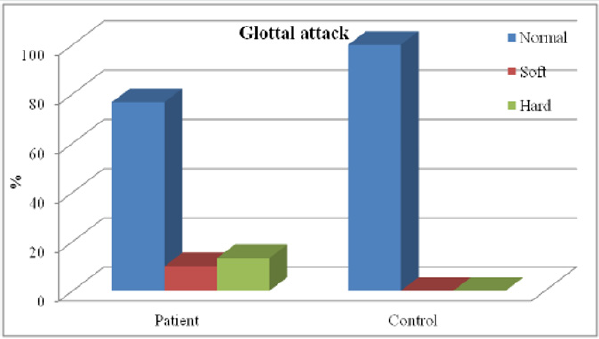
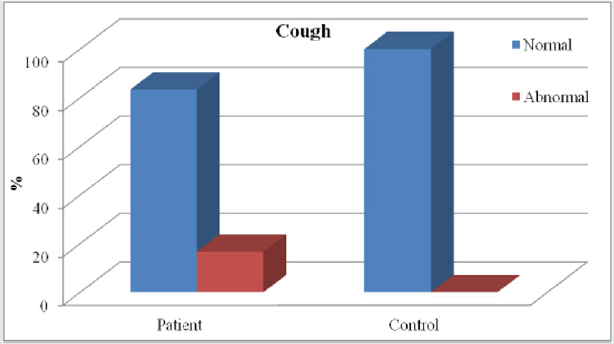
Figure 9: Shows significant difference between the two groups (A&B) regarding cough.
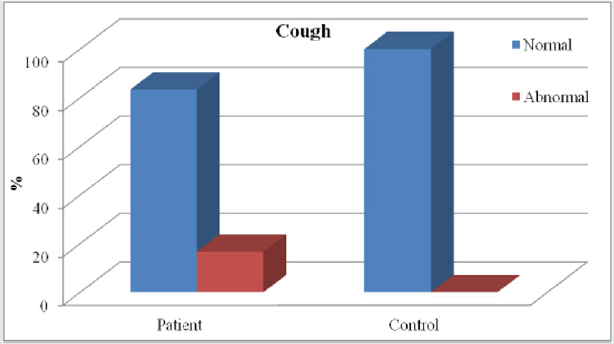
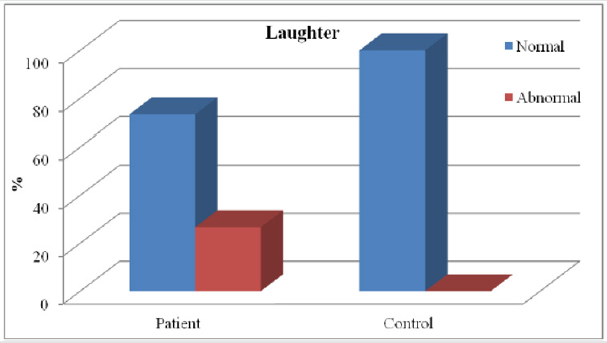
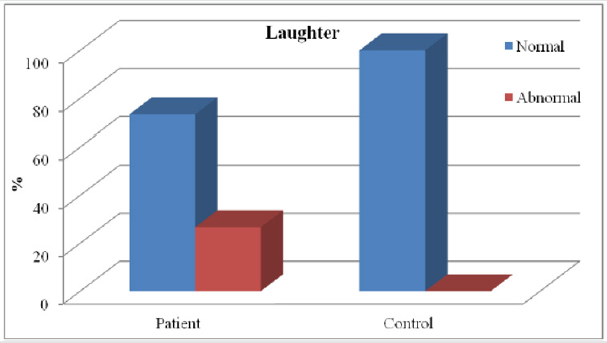
Figure 10: Shows highly significant difference between the two groups (A&B) regarding laughter.
Discussion
Voice is central to a wide range of human activities, and it’s
an audible sound by phonation which is the physical act of sound
production by mean of vocal fold interaction with the exhaled
air stream. A voice disorder exists when a person’s quality, pitch
and loudness of voice differ from those of persons of similar age,
sex, cultural and geographic background [9]. Several studies had
examined voice changes in patients following thyroidectomy, but
there was a lack of studies that determined changes of vocal quality
prior to thyroidectomy, Their for the purpose of our study was to
identify auditory perceptual changes in voice for those with thyroid
disease pre-operatively and determine how these changes differed
from a control group. Results of this current study showed that
86.7% of thyroid patients were females and these results were in
agreement with [10]. who suggested that the prevalence of thyroid
disease is (3.0 to 9.0%) of population with percentage (80% females
and 20% males) which was explained by thyroid disease may be
an autoimmune disease (Hashimoto thyroiditis),which is common
in females with prevalence rate 4:1 female to male, also thyroid
diseases are hormonal dependent so they are common during
pregnancy. Also, these results were in agreement with [11]. They
made a study involved an evaluation of 96 participants with thyroid
or parathyroid disease who were referred to speech pathology by
Otolaryngologists for a pre-operative voice assessment there were
72 (75%) females and 24 (25%) males. Results Showed highly
significant difference between the two groups regarding chewing
and swallowing affection, that 26.7% of patient group were
complaining of chewing and swallowing disturbance with P-value
(0.002). These results were in agreement with [12]. Who studied
patients with thyroid disease pre-operatively and found that (25%)
of patients were complaining of swallowing disorders? Results of
Auditory Perceptual Assessment (APA) by GRBAS.
Modification Showed highly significant difference between the
two groups (A&B) regarding dysphonia, these results showed that
36.7% of patients with thyroid disease were dysphonic with P-value
(0.001) and these results were in agreement with [4] who had a
study which examined patients before and after thyroidectomy,
they used Visipitch (Kay Pentax, Lincoln Park, NJ) to measure
levels of dysphonia. They also used a subjective questionnaire
after surgery to determine the patient’s view on their voice. Onethird
of their patients (15/44) presented with dysphonia before
surgery and 22% reported voice abnormalities after. According to
their findings, patient reported dysphonia matched the dysphonia
recorded with Visipitch with only 64% accuracy. They also used a
subjective questionnaire after surgery to determine the patient’s
perception of their voice. High significant difference between the
two groups (A&B) regarding the Grade of dysphonia were showed
in the results which showed that (16.7%) of patients with thyroid
disease had mild degree of dysphonia, also (16.7%) had moderate
degree of dysphonia and ( 3.3%) had sever degree of dysphonia.
These results were also founded by [13]. Who found that (19.2%)
of patients with thyroid disease had mild degree of dysphonia, also
(14.1%) had moderate degree of dysphonia and (2.2%) had sever
degree of dysphonia? Explaining that the majority of cases about
(89%) diagnosed with thyroid disease being multinodular goiter,
hypothyroidism, and thyroid nodule which had mild to moderate
effect on vocal performance, however only (11%) of cases diagnosed
as cancer thyroid which usually infiltrating the vocal folds resulting
in sever changes in vocal performance. In the current study patients
with thyroid disease showed a high significant difference between
them and the control group in the character of voice about one third
of patients (11/30) showed changes in voice quality which became:
( breathy, strained or strained leaky), breathy voice was(3.3%),
strained voice was(10%) and strained leaky voice was(23.3%).
These results agree with the results obtained by [14]. In the
study that involved an evaluation of 96 participants with thyroid
disease who were referred to speech pathology by otolaryngologists
for a pre-operative voice assessment. They found that (29.6%) of
cases with strained and/or leaky character and (5.3%) of cases
were breathy in character. There are many premorbid conditions
which can affect the voice but are often disregarded in the context
of dysphonia before a thyroidectomy procedure [15]. Performed
a study which looked at different conditions that affected voice
quality using the Dysphonia Severity Index (DSI). They found
smoking had an effect on the DSI of patients. Their studies showed
patients who had smoked had worse DSI scores and this remained
true 6 months postoperatively. Their study also illustrated scores on
the DSI tended to be predictive of voice abnormalities after surgery
for the first 6 months. Patients who had smoked could potentially
have a more resilient voice abnormality because they showed a
worse score initially and a decreased score after surgery. Smoking
and other forms of poor vocal hygiene can contribute to dysphonia.
But the present study results disagree with results obtained by
[16] and showed that the voice of patients were examined before
surgery as well Laryngostroboscopy was used to visualize the
vocal folds, the voices were recorded and the Multi-Dimensional
Voice Program (Kay Pentax) was used for assessment. Showed no
significant deterioration in the character of voice. This study used
objective measurements in their data collection but did not assess
the patients’ or clinicians’ opinions on the voices. Voice quality can
be affected in patients with thyroid disease, including loss of vocal
range, vocal fatigue, and low speaking fundamental frequency
(Especially in women), hoarseness, coarse and gravelly vocal
Symptoms, weak voice, breathy quality, reduced Intensity and
changes to the singing voice [2]. Results showed that one third
(10/30) of patients with thyroid disease had low pitched voice.
These results explained by [3] as hypothyroidism or underactive
thyroid hormone production reduces tissue fluids throughout
the body, This loss of fluid may affect the health and physiology
of hair, skin, and organs .With respect to vocal symptoms, the
larynx often loses fluid in the lamina propria, as the deeper layers
experience edema, due to these physical changes patients may
experience voice changes such as lower pitch. These results agree
with the results obtained by [17] that performed a study of 395
patients which utilized pre-surgical data. Their study focused on
subjectively reported dysphonia before the surgery, the patients
and their families were presented with a questionnaire which
asked for a perceptual assessment of the voice, whether it was
normal or not classified based on hoarseness, low in pitch, or prone
to fatigue. 30% of patients reported with voice abnormalities such
as low-pitched voice and leaky voice. Results showed no significant
difference between the two groups regarding register. These
results agree with the results obtained by [18] that used a variety
of methods to assess the vocal condition of patients with thyroid
disease allowed for a more complete picture of the characteristics
of a patient’s voice.
Found that there were no changes in register. Results showed
highly significant difference between the two groups regarding
loudness with P-value (0.001) showed that one third (10/30) of
patients with excessively soft loudness. These results agree with
[4] they found that One-third of their patients presented with
excessively soft loudness before surgery, also these results agree
with [18,19] They found that patients with thyroid dysfunction had
excessively soft loudness. The changes in voice loudness explained
by [3] that proved that hyperthyroidism changes affect voice stability
and loudness. But the current study results didn’t agree with results
obtained by [14] that applied auditory perceptual assessment for
96 patients with thyroid disease pre-operatively and found that
there were no significant changes in patients’ voice loudness.
Current study results showed significant difference between the
two groups regarding glottal attack, showed that (10%) of patients
with thyroid with soft glottal attack, and (13.3%) of patients with
thyroid with hard glottal attack that with P-value (0.019), which
disagree with results obtained by [14] who found that no significant
changes in glottal attack with P value (0.932) using Kruskal-Wallis
test which is a non-parametric test used to compare several
independent groups. [20] evaluated patient-reported and clinician
determined voice assessments for identifying post thyroidectomy
dysphonia, Patients were evaluated using patient-reported
symptoms (Voice Case History [VCH]), patient-perceived voice
handicap (Voice Handicap Index [VHI]), clinician-perceived voice
deficits (CAPE-V) and video laryngoscopy (VLS) . The purpose of the
study was, “To examine the utility of patient reported and
cliniciandetermined
voice assessment in identifying post thyroidectomy
voice dysfunction. Fifty military health beneficiaries scheduled to
undergo thyroid resection were included in the study. Persons with
preoperative laryngeal dysfunction or prior neck/thyroid surgery
were excluded. Participants were evaluated preoperatively and 3
times postoperatively (1-2 weeks, 3 and 6 months). There are cases
of postsurgical dysphonia which present without any damage to the
laryngeal nerves.
Most of the literature on post-thyroidectomy dysphonia
provides examples of dysphonia without damage to these nerves
[16]. There are many other potential causes of postsurgical
dysphonia: complications and bruising from endotracheal
intubation, edema of the Laryngeal complex, trauma resulting
from the surgery itself, localized neck pain, dysfunction of the
cricothyroid muscle, psychogenic dysfunctions. Finally, the current
results are going with our hypothesis that patients with thyroid
disease have changes in vocal quality prior to thyroidectomy.
Conclusion
There continues to be a percentage of patients who undergo
thyroidectomies and develop post-surgical vocal disturbances
without any obvious causes, one consideration to explain these
post-surgical rates of dysphonia is to determine if pre-surgical
levels of dysphonia exist in these patients. If surgeons can screen
for pre-surgical dysphonia, the rate of indeterminate postsurgical
dysphonia may be reduced, or at least explained and prepared
for. The perceptual measure of voice by modified GRBAS, revealed
significant differences in (overall grade of dysphonia, pitch,
loudness, register of voice) in a manner that can be considered as a
sensitive and reliable tool of assessment.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/