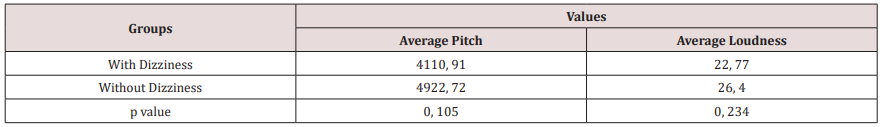
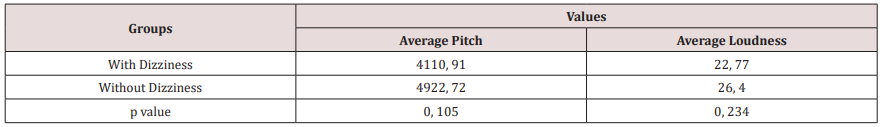
Lupine Publishers | Journal of Otolaryngology
Introduction: Dizziness is a regular complaint, often
accompanied by other symptoms, especially tinnitus. Tinnitus is one of
the three major otoneurological manifestations, alongside neurosensorial
hearing loss and dizziness, being it, most of the times, the
main complaint among patients. The relationship between the vestibular
and cochlear system it’s rather known, many pathologies
can originate from one of both systems.
Objective: Investigate the correlation between the symptoms of tinnitus and dizziness, analyzing the level of disturbance, the
sensation of frequency (pitch) and intensity (loudness) of the tinnitus with dizziness complaint.
Methodology: A descriptive, observational and quantifying field study took place. 126 individuals with tinnitus complaint,
from both sexes, were studied. The anamnesis was performed approaching audiological symptoms, the THI questionnaire was
applied, as well as acuphenometry.
Results: 71 individuals (56,3%) referred to dizziness
complaints associated with the tinnitus; women represented a larger
number (41,3%) (p=0,017). In regards of the level of disturbance of the
tinnitus, most of the patients 18,3% presented a low level,
as for patients without dizziness 14,3% the quick level was present; the
average Pitch is around 4.000 Hz in both groups, Loudness,
on the other hand, was of 22 dBNS for individuals with dizziness and 26
dBNS for individuals without dizziness complaints.
Conclusion: Meaningful results, regarding the relationship between
tinnitus and dizziness, were not observed, therefore, it’s
necessary to investigate if the tinnitus is from vestibular origin in
order to seek improvements to the dizziness and thereafter, the
tinnitus.
Keywords: Dizziness; Tinnitus; Audiology; Speech Therapy
Introduction
The corporal balance relies on the integrity of the vestibular
system (labyrinth, nerve vestibulocochlear, cores, paths and
interrelations
of the central nervous system), somatosensorial system
(receptors, sensors located on tendons, muscles and articulations)
and vision [1]. The labyrinth is responsible for the balance and
position of the body in location. Dizziness and/or imbalance cometo be
when there is interference, both central and peripheral, in the
regular operation of the body balance system. [2]. Dizziness can be
defined, according to the Hearing and Balance Committee of the
American Academy of Comitê de Audição e Equilíbrio da Academia
Americana de Otolaryngology and Head/Neck Surgery [3], as
every and any illusory feeling of motion without any real motion
in relation to gravity. In the practice clinic, it’s one of the most
frequent complaints. It affects between 20% and 30% of the general
population, considering the epidemiological study of Neuhauser
and collaborators [4]. In Brazil, an epidemiological study, performed
in the city of São Paulo, showed that 42% of the individuals
presented dizziness [5]. Occurrences can be found among any age
range, from the first months of birth to the elderly population [6].
Causes can be many, such as: benign paroxysmal postural vertigo
(VPPB), vestibular neuritis, Ménière’s disease, peristaltic fistula,
circulatory, metabolic, hormonal or immunological, cervical spine
changes, head trauma and psychoactive disorders, are one of the
most common. This way, the symptoms coming from the dizziness
may or may not originate from the vestibular system and comprises
sensations described in many ways: vertigo (rotatory dizziness),
imbalance, fluctuation or instability, presyncope our lipothymia,
kinesis (motion sickness), oscillopsia, falling [7]. Dizziness of
nonvestibular
origin are often ill-defined, most of the times they are
labeled as uneasiness, light-headedness, sensation of fainting. Also,
in rare cases, they might represent symptoms of the central nervous
system and/or may be associated with exclusively ocular disorders,
ischemic episodes, metabolic disorder, neurological, cardiac or
cervical diseases [8]. However, dizziness is usually due to primary
or secondary functional disorders of the vestibular system, it might
be classified as rotatory (vertigo – when the illusion of motion
has rotatory characteristics) or non-rotatory (when the illusion of
motion has no rotatory characteristics). Regular vertigo is more
common among peripheral syndromes rather than central ones.
The peripheral vertigo is usually aggravated by eye shutting, unlike
what happens with central vertigo. Both peripheral and central
vertigo can be unleashed or worsen with head motion (this being
the most common kind of rotatory dizziness). On the other hand,
non-rotatory dizziness may be oscillating, hesitant, fluctuance,
wavering, among others. In order to determine the vestibular
source an examination of the alterations of the vestibular system is
required [9]. Dizziness is usually followed by other symptoms; it’s
intensity can cause loss of balance and falls. Normally, the dizziness
appearance is accompanied by neurovegetative symptoms,
megrims, eyesight darkening and lack of concentration.
Dizziness is also highly associated with auditory symptoms,
such as hearing loss, sensation of auricular plenitude and, mainly,
tinnitus [10,11]. The tinnitus is one of the 3 major otoneurological
manifestations, alongside neurosensorial hearing loss and
dizziness, being it, most of the times, the main complaint among
patients, especially elder ones [12,13]. The tinnitus, also known
as tinnitus, can be defined as auditory illusion, in other words,
an endogenous sound illusion, not related to any outside source
of stimulation [14]. The presence of tinnitus might be a factor
of great negative repercussion in one’s life, jeopardizing sleep,
concentration during day-to-day and professional, as well as social
life. Many times, it affects the emotional balance of the patient,
unleashing or worsening states of depression and anxiety [15].
A study performed in the city of são Paulo shows that 22% (430
individuals) present tinnitus [16]. The tinnitus is as symptom
that can be caused by a number of medical conditions: otological
affections, neurological, cardiovascular, metabolic, pharmacologic,
odontological, psychologic, side effects of medications and possible
drug ingestion, such as caffeine, nicotine and alcohol [17]. Up to
date theories to explain the source of tinnitus defend the hypothesis
that it occurs due to anomalous and spontaneous neural activity
in the central pathways, auditory or not, being a consequence of
sensory deprivation, aftermath of cochlear lesion [18,19]. The
description of the tinnitus’s characteristics might vary from patient
to patient, from “pure tone” sound to a “whistle”, a “noise” or even
a “whisper”, etc. Perceivable in one or both ears, and yet in the
head, with no specific side. It can be constant or intermittent, being
absent for some periods of time. Its intensity may vary from light
to very intense [18]. Patients with dizziness, resistant to various
treatments, can be as hard to conduct as patients with high level
of tilllindus disturbance, these that might happen simultaneously
or independently. Both dizziness and noise are extremely common
symptoms at the practice clinic, as shown by the study performed
by Moreira and collaborators [20] where out of 27 individuals
affected by dizziness, 16 (59,2%) also complained about noise.
The relationship between the vestibular and cochlear systems
is rather known. Many pathologies may originate in one of those
systems or simultaneously, as well as having one of them as
primary source due to influence in other systems functionality.
Therefore, it’s possible that changes in the posterior labyrinth
(Semicircular Canal) fluids may cause tinnitus [21]. It’s noticeable
that both disorders jeopardize the individual’s quality of life. The
tinnitus may affect one’s sleep, concentration, emotional balance
and social life. On the other hand, dizziness, apart from other
mentioned symptoms, might hinder the individual’s performance
during activities that require quick head motions and, also, tasks
that imply flexing the torso and the head [22]. Innumerable
reports of dizziness among patients with tinnitus complaints
were observed in a Multidisciplinary service of attendance to
patients with tinnitus. The aforementioned research main goal
was to investigate the correlation between dizziness and tinnitus
symptoms on those patients, analyzing the level of disturbance, the
sensation of frequency (pitch) and intensity (loudness) of tinnitus
with dizziness complaint.
Material and Methods
The present study was performed in one School Clinic of the
Speech Therapy Course located in João Pessoa. 126 individuals
with tinnitus complaint were evaluated, 81 females and 45
males, ages ranging from 17 to 83 years old, all attended in the
Multidisciplinary Tinnitus Service. It was a descriptive research.
As for technical procedures, a field study is more fitting, as it tries
to deepen between the dizziness and its relationship towards
tinnitus. In order to validate these hypotheses, a transversal and
observational study, of quantitative characteristics, was performed.
In accordance with the 466/12 Resolution of the National HealthCommittee, referring to ethics regarding research that involves
human subjects, the study was approved by the Ethics in Research
with Human Subjects Committee (prot. N. 0129/12). Clearance was
obtained through the signing of the Term of Free and Enlightened-
TCL by volunteers and/or responsible for the project. All patients
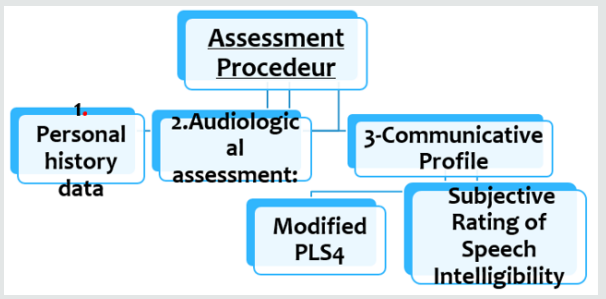
were subjected to the following procedures:
I. Answering anamnesis questions which emphasize the
patient’s auditory symptoms, in order to collect personal data of
the individual; data about the tilllindus - location of the tinnitus
(right, left, in the head or undetermined), time of onset, how it
came to be (gradual, sudden, after noise exposure, other), kind
(continuous, pulsatile, intermittent), characteristics (whistle,
rain, noise, waterfall, bee, other); and other possible associated
symptoms, such as dizziness.
II. In order to obtain more directed information regarding
the patient’s tinnitus, the Tinnitus Handicap Inventory (THI)
questionnaire was applied, as an interview. The THI is a
questionnaire that evaluates the severity of the tinnitus, with 25
questions approaching three dimensions: nine questions related
to emotional aspects (frustration, anger, irritability, anxiety,
depression and insecurity); eleven questions related to functional
aspects (stress, concentration, sleep, workplace interference,
house responsibilities and social activities); antivideos socials);
and five questions related to the catastrophic aspects (despair,
lack of self-control, inability of acceptance, perception of terrible
illness) (Lim et al, 2010). Those 25 questions allow the following
possibilities of answer: “yes”, “no” and “sometimes”, each having
a score of “4 points”, “0 points” and “2 points”, respectively. This
said, each question will add points to its category, be it functional,
emotional or catastrophic, and the total sum, varying from 0 to a
100. Depending on the result, the level of disturbance caused by the
tinnitus might be classified as, by the total sum, as:
a) LEVEL 1 (Quick): Score 0 - 16. Only perceived in quiet
environments.
b) LEVEL 2 (Light): Score 18 - 36. Easily masked by
environmental and easily forgotten during day-to-day activities.
c) LEVEL 3 (Moderated): Score 38 - 56. Perceived in the
presence of background noise, however, day-to-day activities can
still be performed.
d) LEVEL 4 (Severe): Score 58 - 76. Almost always perceived,
leads to disturbance in sleep patterns and may interfere in daily
activities.
e) LEVEL 5 (Catastrófico): Score 78 - 100. Always perceived,
sleep patterns disturbances, difficulty performing daily activities.
Later on, acuphenometry was performed in order to obtain
data regarding the sensation of intensity (loudness) and frequency
(pitch) of the tinnitus. The test took place in an acoustic cabin, using
the audiometer model AVS 500, of the Vibrasom brand. To unilateral
tinnitus, the sound was supplied to the contralateral ear and, if
bilateral, to the ear with best hearing [23]. In order to identify what
kind of tinnitus, the Pure Continuous Tone, Pulsatile Pure Tone and
Modulated Frequency were presented, in audible intensity, so that
the patient could choose which resembles his own tinnitus more.
To measure Pitch, the chosen tone was presented in frequencies
ranging from 125 to 8000 Hz. And to investigate loudness, the same
tone was presented in the frequency identified by the patient, with
audible intensity, incrementing 1 db.
Data Analysis
The data was registered in an Excel spreadsheet for further
analysis. Initially, a static descriptive analysis was performed, in
order to verify the frequency of the variables studied (tinnitus,
dizziness, age, gender).
As it follows, the inferential static analysis was also performed,
with the help of adequate tests, in order to verify:
a) The correlation between variables: Spearman Correlation
test aiming to verify the level of relationship between pairs
of variables of interest, such as THI x Dizziness, Gender x
Dizziness.
b) Comparison between pitch and loudness values to each
group, with or without dizziness: parametric test t of Student
to independent samples of interval variables of normal
distribution; or its nonparametric correspondent when needed.
c) The differences were considered meaningful when p0,05
was presented. The static analysis was performed through the
Software Statistical Package for Social Sciences (SPSS), version
20.0.
Results
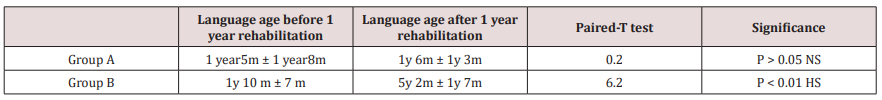
Out of the 126 evaluated individuals (64.3%) are female and 45
(35.7%) male, with average age of 49,33 years. All of them presented
tinnitus, whom 71 (56,3%) also complain about dizziness, whereas
55 (43,7%) don’t. Based on this, it was noticed that most part of the
studied population stated complaints regarding tinnitus associated
dizziness, also the static analysis shows that the variable gender
has great interference in the presence or absence of dizziness.
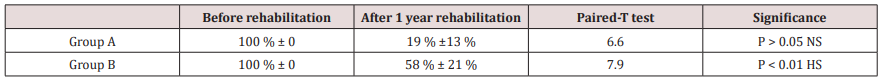
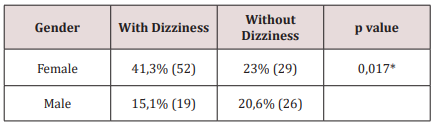
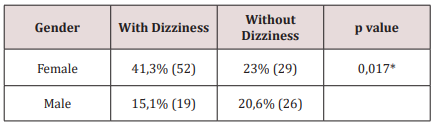
Regarding the THI questionnaire, the patients with dizziness
presented bigger results for the light level, however patients
without dizziness, presented bigger results to the quick level. As
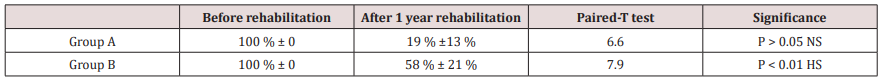
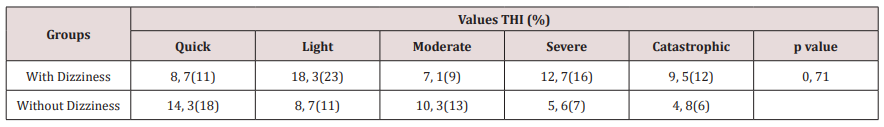
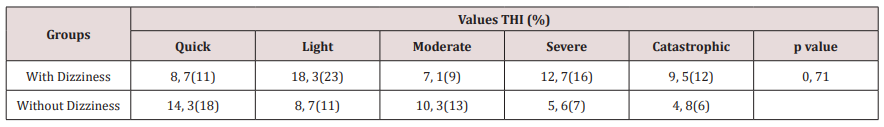
for tinnitus characteristics, both groups presented average pitch
around 4.000 Hz, with no meaningful statistical difference between
them. On the other hand, loudness average of the tinnitus was
22 dBNS for the dizziness group and 26 dBNS for the individuals
without dizziness, no meaningful difference between the groups
was found (Tables 1-3).
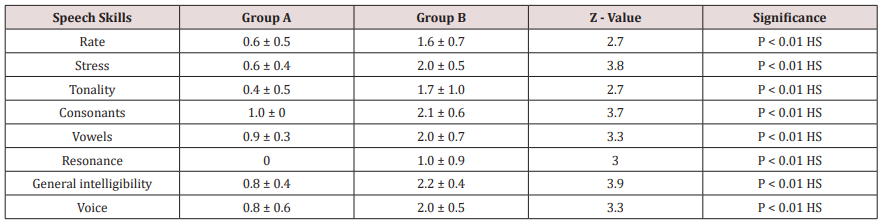
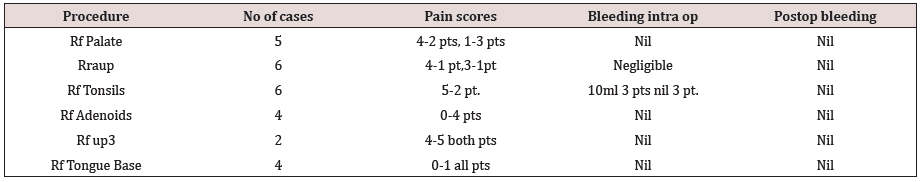
Table 1: Descriptive and inferential statistics of the variables
gender and dizziness.
Meaningful difference (p<0,05) according to Spearman’s
correlation test.
Table 2: Descriptive and inferential statistics of tinnitus disturbance and dizziness.
Meaningful difference (p<0,05) according to Spearman’s correlation test.
Table 3: Averages of pitch and loudness of the tinnitus.
Meaningful differences when p<0,05 according to the t Student test.
Discussion
Both tinnitus and dizziness are otoneurological complaints
often presented at the practice clinic. Patients that exhibit tinnitus
might also show signs of alteration and/or vestibular complaints.
In this research, was observed that most of the population filed
dizziness complaints. This data corroborates with literature,
seeing it as complaint usually reported alongside tinnitus [20,21].
Data from table one shows that more women (41.3%) presented
complaints about dizziness associated with tinnitus and there
was a meaningful correlation (p=0,017), in accordance with what
literature shows [24-27]. It is believed that the higher occurrence
among females might be due to factors such as: variation of the
hormonal cycle, higher occurrence of migraines and the fact that
women are more likely to seek medical attention [27,28]. Therefore,
the variable gender directly affects the presence or not of dizziness.
The disturbance caused by the tinnitus may vary greatly, and
there are factors that appear to be associated with a higher level
of disturbance, such as stress, psychiatric disorders and gender
[29,30]. The THI analysis, expressed in table 2, showed that most
of the patients with dizziness presented light level 18,3%, whereas,
patients without dizziness presented the quick level 14,3%.
Therefore, the data is compatible with the ones presented by the
studies of Xavier [31] and Lim et al. [32] that highlight the light and
quick level as the most common among the samples of tinnitus. It
can also be observed in the present study that, despite the variables
THI and Dizziness lack of meaningfulness (p= 0,71), patients with
dizziness complaints seem to exhibit a higher level of disturbance
regarding tinnitus than the ones without complaint. In regards to
the characteristics of the tinnitus evaluated by acuphenometry
(Table 3), when compared to frequency values, both groups showed
an average pitch around 4.000 Hz, in other words, the two groups,
regardless dizziness complaints, exhibited the pitch of the tinnitus
in acute frequencies, with no meaningful statistical difference
between them (p=0,105). These findings are in accordance with the
studies of Urnad and Tochetto [33] and Suzuki and collaborators
[34] which also verifies values referring to the tinnitus’s pitch in
acute frequencies.
This is strongly related with the fact that most patients with
tinnitus present hearing loss in these frequencies. The researchers
state that there is a connection between the tinnitus’s pitch and
the region of the frequency of the maximum hearing loss. Taking
intensity into consideration, the average loudness of the tinnitus
was 22 dBNS for the group with dizziness and 26 dBNS for
individuals without it, no verified meaningfulness between the
two groups (p=0,234). This data goes against the values of the
studies of Buzo and Carvallo [35] and Tugumia and collaborators
[36] that verified loudness varying from 5 to 15 dBNS, this way, our
population shows a bigger sensation of intensity to the tinnitus.
Meaningful results regarding the relation between tinnitus and
dizziness were not observed in this sample. Probably, the dizziness
complaints of these patients are not related to the vestibular
system and, consequently, to the tinnitus. Understanding that the
auditory and vestibular systems are intimately related, it becomes
necessary that the patient with dizziness complaints be directed
to and otoneurological evaluation, in order to investigate if the
source of dizziness is vestibular, what could possibly strengthen the
relationship between the tinnitus and the dizziness. Afterwards, it
is possible to seek treatment in order to improve both conditions,
simultaneously, as it is for vestibular rehabilitation which is used as
a therapeutic process for dizziness when associated with tinnitus,
possibly decreasing the level of disturbance caused by the tinnitus,
as in accordance with the study presented by Zeigelboim and
collaborators [37].
Conclusion
Based on the results found in the researched sample:
a) Most of the patients with tinnitus presented dizziness
[38].
b) The variable female gender showed meaningfulness
regarding the presence of dizziness.
c) An average pitch of around 4.000 Hz was found for
individuals with and without dizziness.
d) Average loudness was 22 dBNS for individuals with
dizziness and 26 dBNS for individuals without.
e) The level of disturbance of the tinnitus showed no
meaningfulness/relationship with dizziness.
For more
Lupine Publishers Open Access Journals Please visit our website: h
http://lupinepublishers.us/For more
Journal of Otolaryngology-ENT Research articles Please Click Here:
https://lupinepublishers.com/otolaryngology-journal/