Abstract
Background: The use of cochlear implantation (CI) can
fully restore hearing. Consequently, speech production can improve
over time and enters the normal rang when traditional amplification
Devices (hearing aids) are unable to restore access to the full
range of phonemic components of speech, a cochlear implant (CI) is a
widely used treatment option for children with sensorineural
hearing loss (SNHL).
Purpose: The aim of this study is to compare the
functional benefit of the communicative skills of children with CI
without
pre-implantation aural/oral rehabilitation in relation to those with CI
with pre-implantation 6 months aural/oral rehabilitation in
order to compare the role of pre-implantation aural/oral rehabilitation
on the communicative abilities of severe to profound and
profound sensorineural hearing impaired children.
Method: This study has a prospective design. It started
after final diagnosis and decision that all children are candidates for
CI
but half of them are fitted with behind the ear hearing aids and the
other half of children are immediately implanted provided that
the primary language assessment before rehabilitation is present in the
medical files of these children. A 2nd language assessment
was done after 12 months of language therapy to detect the progress of
the language development. These sixty patients were
divided into two groups:
a) Group A: Thirty children, who have used behind the ear hearing aids for one year before CI and attended regular language
therapy.
b) Group B: Thirty children, who shifted immediately to cochlear implantation, and were enrolled in auditory training and
language therapy for one year.
Results: Total language age of children using cochlear
implant without pre-implantation aural/oral rehabilitation is
significantly
higher than that in the children while using hearing aids for one year
before CI. Also, there is highly significant difference between
frontal and back speech sounds in the children after immediate
implantation with positive correlation.
Conclusion: Cochlear implant is safe & reliable technique. The fact that many profoundly hearing impaired children using
immediate cochlear implant without pre-implantation aural/oral rehabilitation can develop functional levels of speech perception
& production, develop competency level in a language other than their primary language and continuation of language therapy
together with proper mapping accordingly is a must to enroll these children in main stream education.
Keywords: Hearing Aids; Cochlear Implant; Language; Speech Intelligibility Pre-implantation Rehabilitation
Abbreviations: SNHL: Sensorineural Hearing Loss; HA: Hearing Aids; CI: Cochlear Implantation
Introduction
Language in children begins to develop since birth and is nearly
complete by the age of 6 years. Language skills, speech quality,
expressive and receptive vocabulary are enhanced by exposure to
aural language since as early an age as possible [1]. Children spend
many hours in acoustic environments where target speech signals
are embedded in competing sounds from multiple sources. In these
environments, perception of target speech is assisted by a listener’s
a listener’s ability to segregate the multitude of sounds into separate
auditory streams, one cue to which is the angle of incidence of
different sounds [2]. Children with profound sensorineural hearing
loss (SNHL) experience delays in learning to understand the speech
of others and to produce intelligible speech. There is solid evidence
that moderate (or more severe) hearing impairment exerts a
negative impact on speech, language, cognitive development,
and early identification and management may be of great benefit
to these children, through improved language, communication,
mental health, and employment prospects [3]. The use of Hearing
Aids (HA) or Cochlear Implantation (CI) can partially or fully
restore hearing. Consequently, speech production can improve
over time and enters the normal range. After hearing is restored,
hearing impaired individuals use auditory feedback to adjust voice
features such as voice intensity, intonation and vowel duration [4].
When traditional amplification devices (hearing aids) are unable to
restore access to the full range of phonemic components of speech,
a cochlear implant (CI) is a widely used treatment option for
children with SNHL [5]. Cochlear Implants (CI) which are called as
bionic ears are effective in trans- mitting salient features of speech,
especially in quiet [6]. Because the goal of restored hearing in a
deaf child is to enable useful hearing, a key measure of outcome
should reflect how a deaf child’s experience with a CI develops into
the effective use of spoken language. Parental surveys indicate that
the outcome of their greatest concern after surgical intervention in
children with SNHL is the level of spoken language achieved [7].
Cochlear implants have become a popular option for children with
profound hearing loss. Evidence supporting the benefits of early
implantation is found in experimental [1], developmental [2], and
clinical cochlear implant studies [3]. The consensus is that children
have the best opportunity to learn language during their first 5 years
of life. According to [2], this critical period for language learning
is particularly important in deaf and hearing-impaired children.
Providing cochlear implants to deaf children at a young age may
enable them to take advantage of this critical period for learning
language and is likely to increase their chances for developing
speech and language skills like those of normal-hearing children.
Early implantation would also result in a decrease in the duration of
auditory deprivation, a decrease considered to positively influence
performance with a cochlear implant [4].
Objectives
The aim of this study is to compare the functional benefit of the
communicative skills of children with immediate CI without preimplantation
aural/oral rehabilitation in relation to those using
hearing aid with pre-implantation aural/oral rehabilitation in order
to compare the role of each amplification device and the effect of
pre-implantation aural/oral rehabilitation on the communicative
abilities of severe to profound and profound sensorineural hearing
impaired children.
Subjects & Methods
This research was conducted during the period between the
years 2017 and 2018. The study protocol was approved by the
Otolaryngology Department Council of Beni-Suef University and
Otolaryngology Department Council of King Abd Elaziz specialized
hospital Jouf, Saudi Arabia. Consent to participate in this research
was obtained from the subjects’ parents before commencement of
the study. This study employed a comprehensive design to examine
outcomes in multiple domains of communication in children
who used either bilateral behind the ear hearing aids and preimplantation
aural/oral rehabilitation or an immediate unilateral
cochlear implant without pre-implantation rehabilitation for a
period of one year. These were selected from children seeking
language rehabilitation in Phoniatrics Unit, Beni-Suef University
Hospital and children seeking language rehabilitation in Phoniatrics
Clinic, King Abd Elaziz specialized hospital Jouf, Saudi Arabia.
Shortly after confirmation of bilateral permanent hearing loss, thirty
children were typically fitted with bilateral behind the ear hearing
aids using the desired sensation level (DSL) prescription method
and regularly attend aural/oral rehabilitation sessions. Thirty
children underwent a comprehensive team evaluation for cochlear
implant candidacy and received immediate unilateral cochlear
implants without pre-implant aural/oral rehabilitation. All children
received audiologic management and preschool rehabilitation
and all children were enrolled in rehabilitation programs with
a focus on the development of receptive &expressive language.
Children were regular in Phoniatrics clinic, were asked to follow
up auditory rehabilitation & language therapy program twice per
week. Children with cochlear implants were followed every month
for mapping of their speech processor and speech recognition
testing. The study received ethical approval from the Hospital of
Beni-Suef University and from King Abd Elaziz specialized hospital
and written informed consent was obtained from all their parents.
Collaboration between ENT clinic, Audiology clinic& Phoniatrics
clinic was done in the form of ENT examination, audiological
assessment, and language assessment and rehabilitation for all
children. This study has a prospective design. It started after fitting
half of the children with bilateral behind the ear hearing aids with
aural/oral rehabilitation sessions and the other half of the children
are immediately implanted, mapped, and regularly attended
aural rehabilitation sessions provided that the primary language
assessment before rehabilitate- ton is present in the medical files of
all children. A 2nd language assessment was done after 12 months
of language therapy to detect the progress of the language and the
efficacy of pre-implantation aural/oral rehabilitation. These sixty
patients were divided into two groups:
a) Group A: Thirty children, who have used behind the ear
hearing aids for one year and attended regular language therapy
despite those children, are candidates for cochlear implants.
b) Group B: Thirty children, who shifted immediately to
cochlear implantation and had regular language therapy and were
enrolled in auditory training.
Half patients were fitted with bilateral powerful digital signal
processing BEHAs and used them for at least a 12-months period
before CI. Hearing aid use was determined by parental and therapist
reports. After surgical implantation of the device and an adequate
healing period for the other half of the patients, the implants were
activated (usually 4 weeks after surgery). The children were fitted
with one of the two brands of speech processors using a behind
the ear controller. Speech processors used in this study were OPUS
2 with standard Sonata electrode & Cochlear Freedom Processor
with nucleus 24 k straight electrode.
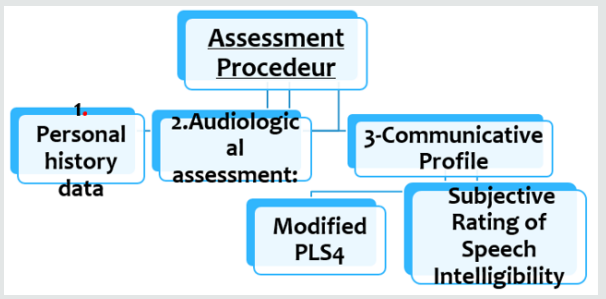
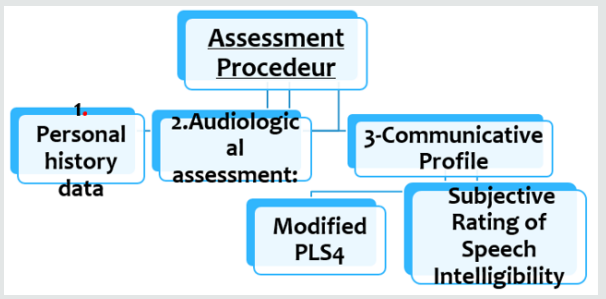
In this study using Modified Preschool Language Scale &
Subjective Speech Intelligibility Test gave us a summary of the
improvement of these children. This is matched with other studies
which focused that both comprehension and expression of spoken
language are important markers of parent-perceived success of a
CI (Figure 1).
Figure 1
Language Improvement Quotient: The language
improvement quotient [8] was used to compare between the
rates of progress in language in order to overcome the bias of age
matching between the individuals in the study.
Language Improvement = 2nd language age -1st language age
divided by duration of language rehabilitation.
a) A1 refers to language development of group (A) after
using bilateral behind the ear hearing aids for 12 months which is
calculated by this equation:
A1= 2nd language age -1st language age divided by 12(duration
of rehabilitation)
b) B1 refers to language development of group (B) after using
unilateral CI for 12 months which is calculated by this equation:
B1= 2nd language age -1st language age divided by 12(duration
of rehabilitation).
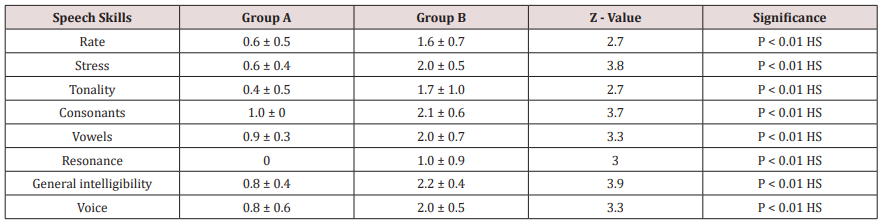
Speech analysis was performed using the Ain Shams
assessment protocol which includes analysis of supra-segmental
phonology (rate, stress and tonality), segmental phonology
(consonants and vowels), nasal resonance and general intelligibility
of speech. Assessment of auditory perception skills was performed
evaluating a hierarchy of listening skills ranging from detection,
to discrimination, identification, recognition and comprehension.
Assessment of speech reading abilities was done and expressed as
percent change over time.
Statistical Studies
Data was analyzed using SPSS, Statistical Package for the
Social Sciences version 17 (SPSS Inc., Chicago, IL). Numerical
data were expressed as mean, standard deviation, and range. For
quantitative data, comparison was done using Mann-Whitney
test (non-parametric t-test). A p-value < 0.05 was considered
significant. Spearman-rho method was used to test correlation
between numerical variables (r > 0.3 = no correlation, r = 0.3-0.5 =
fair correlation, r = 0.5-0.1 = good correlation).
Results
Group (A) are hearing aids users for one year, Group (B) are CI
users for 1 year. Demographic data of the 2 groups:
a) Age
b) Gender.
c) Incidence of hearing loss.
d) Psychometric evaluation.
e) Pure tone Audiometry.
f) First language age.
g) Radiology.
a) Age Distribution: Both groups are matched according
to age. In group (A) the age of the children ranged between 3
years and 7years. In group (B). The age of the children ranged
Between 3 years & 7 years, provided that all children were
implanted before the age of 6 years.
b) Gender: No significant difference was noted in gender of
both groups.
c) Incidence of Hearing Loss: In group (A) there were
24 children (80%) with congenital hearing impairment and
6 children (20%) with acquired hearing loss, while in group
(B) there were 18 children (60%) with congenital hearing
impairment and 12 children (40%) With acquired hearing loss.
d) Psychometric Evaluation: All children in group (A)
had normal psychometric evaluation with a mean Value 87.5±
4.6; also, in group (B) all children had normal psychometric
Evaluation with a mean value 86.4±5.1.
e) Pure Tone Results: Pure tone results of group (A)
maintained a mean value of 27.9 dB HL. Group (B). Decreased
in mean values from 65.7±8.2 dB HL. There was a highly
significant difference (P=0.001) between group (A) and group
(B) in favor of group (B).
f) First Language Age: Before start of therapy, both groups
had no passive vocabulary and were Nonverbal. They used
either babbling or vocal play.
g) Radiology: All Children both in groups (A) and (B) were
having normal CT and MRI of Petrous bone.
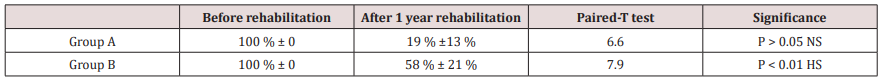
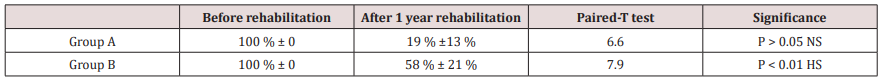
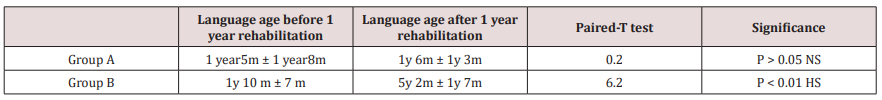
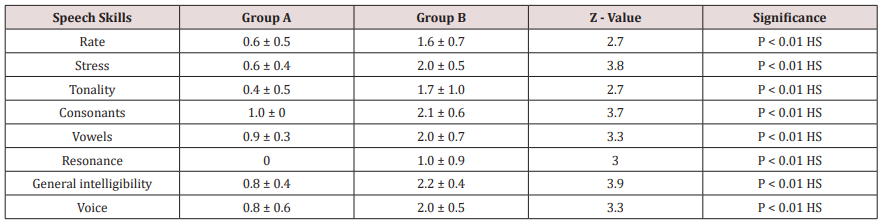
Tables 1-3 demonstrate the progress of the language abilities,
the auditory abilities and the speeding reading abilities of both
groups, respectively, from the time just prior to the rehabilitation
(either oral\ aural in group A or aural in group B) as compared to
the evaluation done one year the rehabilitation (Table 4).
Table 1: Results of collective language improvement in both groups using paired-T test.
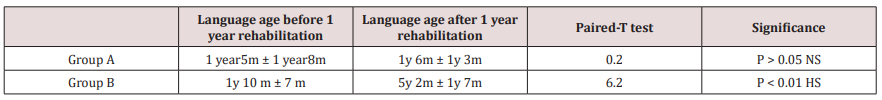
Table 2: Results of progress in speech reading ability before and after rehabilitation in the 2 groups (using Paired-T test).

Table 3: Difference in the speech ratings between the 2 groups after 3 years of rehabilitation (using Mann-Whitney test).
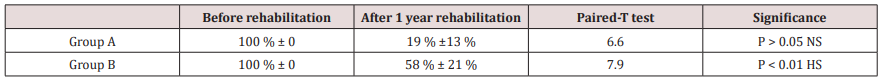
Table 4: Results of collective language improvement in both groups using paired-T test.
Discussion
The primary purpose of this study was to obtain comprehensive
data on the development of language and speech skills in a group
of permanent hearing impaired children. This group shared the
common degree of bilateral hearing impairment (severe to profound
or profound hearing impairment), they all sought amplification, and
they all sought language rehabilitation after receiving amplification
using primarily auditory-based cues. The study aimed also to
investigate the difference between the language and speech
development under two amplification conditions; bilateral behind
the ear hearing aids and unilateral cochlear implants. The choice of
language age deficit to compare language skills development among
the studied groups is justified by the fact that three variables usually
co-vary when language results are analyzed in children; age of use
of the amplification device whether hearing aid (HAs) or cochlear
implant (CI), the language age before start of rehabilitation, and
the language age of children after the time of rehabilitation. The
difference in ages at evaluation places the younger children at a
maturational and developmental disadvantage in comparison with
their older peers. Thus, analyzing the results in terms of language age
scores might put the younger group at a disadvantage. At the
same time, analyzing the results in terms of language age deficits,
although more reasonable, but still, in theory, puts the older group
at a disadvantage because of the impact of their ages giving higher
values for the deficit from the scored language age. That’s why the
hypotheses of using the language improvement quotient [8] after
determining the exact language age, may be more realistic and less
biased by the chronological age differences at the time of evaluation.
In this study using Modified Preschool Language Scale & Subjective
Speech Intelligibility Test gave us a summary of the improvement
of these children. A perfect model for comparing the results of both
devices may be practically impossible, given the current indications
of cochlear implant use. In this study, which was applied on two
groups with comparable ages, a comparison was made between the
outcomes of the 2 devices along a period of (re)habilitation of one
year in their course of therapy. If the CI group were doing better
than the HA group, it would indicate that the selection criteria
were too conservative and some of the HA users might be better off
with a CI. This raises the suspicion of the fact that HA users plateau
after a period of little progress or at least their progress continue
at a less pace. Cochlear implants may have a superior effect on the
acoustic environment of children more than hearing aids. During
the 90s of the last centuries, and using the early models of speech
processes, studies proved that CI users gained better results than
HA users in language and perception skills [9-14]. The minimum
age for implantation has progressively reduced [15]. Advantages
of cochlear implants over hearing aids extended also the adult
population [15]. In a study by [16], they found CIs and children
with HAs, aged 4 to 5 years, differ significantly on language abilities
and there were differences in articulation skills in favor of the CI
users. Advances in sound processors and related software have
enhanced the fidelity with which complex sounds are processed
into physiologically meaningful codes [17]. This study pointed to
the importance of conducting comprehensive assessments when
evaluating whether a child with severe to profound sensory neural
hearing loss would likely derive greater benefit from a cochlear
implant compared to a hearing aid. To date, only a few systematic
studies have involved large numbers of children who received
implants at various ages and have investigated both the effects of
age at implantation and the amount of experience with an implant.
Most of such studies were concerned with the speech perception
skills after cochlear implantation with a clear evidence of the effect
of early implantation on rate of acquisition of such perception skills
when they are implanted at 2 – 4 years of age [18]. Concerning the
auditory abilities, the progress imposed by the effect of cochlear
implantation group produced better abilities than the hearing
aids group in the auditory abilities. This may be explained by the
fact that the hearing aids group were more rigid to their habits of
relying on their visual cues making the children less efficient in
acquiring the training proficiency provided to them during therapy
sessions. In an explanation of this, [19] described recruitment of
the auditory cortex by the visual and somatosensory systems in
congenitally deaf humans. They reported that the extent of crossmodal
recruitment of the auditory cortex increases as the duration
of deafness increases, deterring the restoration of auditory
processing in the auditory cortex of long-term deafened individuals
after cochlear implantation. They also suggested that the age
beyond which the effects of cross-modal plasticity in the auditory
cortex are more difficult to reverse is about 6.5 years. It has also
been documented that there is a change in the cochlear place code
during development [20]. This may be necessary for the formation
of normal and effective connections between auditory centers and
for the proper development of elements within the central auditory
pathways. Early cochlear implantation may contribute to the
maintenance of these important developmental milestones.
Conclusion
CI children showed better rate of language acquisition skills
along a one-year use of the implant compared to a similar period
of HA group of HA users. The implanted group demonstrated
significantly better auditory abilities, better speech production
skills, and better speech intelligibility one year after implantation
and with aural rehabilitation - than the aided group with oral\aural
rehabilitation. The implanted group also ended with significantly
less or no speech reading abilities than the aided group one year
after implantation. These results indicate the favorable effect
implantation over the previous parameters. Language skills shows
a significant difference between the two groups. Consequently,
oral\aural rehabilitation with hearing aids – even for few monthsis
not mandatory.



No comments:
Post a Comment