Lupine Publishers | Journal of Otolaryngology
Abstract
Introduction: The World Health Organization confirmed COVID 19 as a pandemic on 11th March 2020. Though the most common symptoms of COVID-19 are fever, cough, myalgia, fatigue, and difficulty breathing, ear, nose, and throat (ENT) symptoms, including loss of sense of smell and/or loss of sense of taste have been reported as symptoms caused by the virus.
Aims and Objectives: To detect and discuss the different otorhinolaryngology (ORL) manifestations reported in COVID-19 positive patients.
Materialsand Methods: This observational study was done on 2000 patients with a positive COVID 19 test admitted to a tertiary care hospital. The patients were assessed for their signs and symptoms and the findings were analysed.
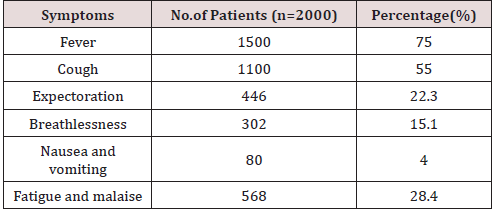
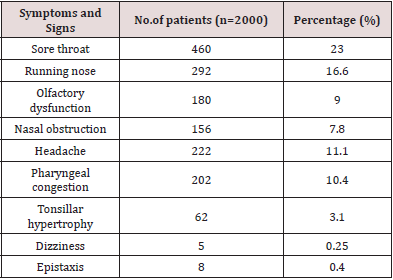
Results: The patients ranged in age from 18 to 70 years, including 1090 males (54.5%) and 910 females (45.5%). The most common presenting symptom was fever seen in 1500 (75%) patients. Other symptoms included cough in 1100 (55%) patients, expectoration seen in 446 (22.3%), breathlessness in 302(15.1%), nausea and vomiting in 80(4%) patients, fatigue/malaise in 568 (28.4%) patients.The most common otorhinolaryngological manifestation were sore throat seen in 460 (23%) patients, running nose in 292 (14.6%), olfactory disturbances in 180 (9%), nasal obstruction in 156(7.8%) , headache in 222(11.1%), pharyngeal congestion in 208(10.4%), tonsillar hypertrophy seen in 62(3.1%) patients.
Conclusion: Though, the most common presenting symptoms in COVID-19 patients are fever and cough, a significant proportion of patients does have ENT manifestations which may go unnoticed. Hence it becomes necessary to screen all COVID patients for ENT symptoms so that high quality care can be provided for patients.This also facilitates care givers to take necessary precautions to protect themselves.
Keywords: COVID 19;otorhinolaryngological; manifestations
Introduction
The Severe Acute Respiratory Syndrome Coronavirus 2 (SARSCoV- 2), firstly known as the 2019 novel Coronavirus (2019-nCoV), started in Wuhan in China in December 2019[1].The World Health Organization confirmed it as a pandemic on 11thMarch 2020[2]. Although this virus can cause severe respiratory failure and even death in infected patients, it has spread rapidly and continues to spread among people because it can cause mild or no symptoms in the majority of cases[3,4].The most common symptoms of COVID-19 are fever, cough, myalgia, fatigue, and difficulty breathing. In addition, ear, nose, and throat (ENT) symptoms, including loss of sense of smell and/or loss of sense of taste have been reported as symptoms caused by the virus.The aim of this study was to detect and discuss the different otorhinolaryngology (ORL) manifestations reported in COVID-19 positive patients.
Materials and Methods
All patients with confirmed reverse transcriptase polymerase chain reaction (RT-PCR)-positive testing for the SARS -CoV-2 viral genome were assessed for symptoms and signs. 2000 patients who presented to a tertiary care designated COVID hospital were included in the study. Health workers with confirmed positive PCR test results were voluntarily enrolled in the study. All subjects provided informed consent to participation in the study.
The inclusion criteria were
a) Patients>18 years of age with a positive COVID -19 test.
b) Patients having mild to moderate symptoms.
The exclusion criteria were
a) Age< 18 years old.
b) No confirmed positive PCR test result.
c) A history of chronic nasal problems.
d) Recent head injury, recent nasal surgery.
e) Severe respiratory failure or treatment in the intensive
care unit.
Results
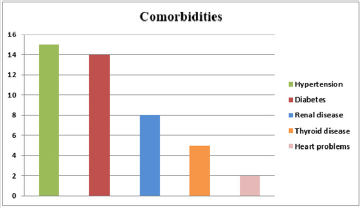
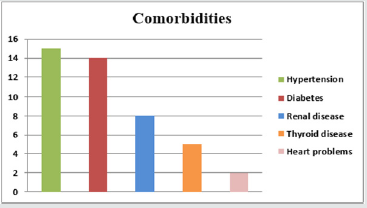
A total of 2000 patients were included in the study. The patients ranged in age from 18 to 70 years, including 1090 males (54.5%) and 910 females (45.5%)(Figure 1& Table 1).The most prevalent comorbidities in these patients were (Figure 2& Table 2).
a) High blood pressure in 15%,
b) Diabetes in 14 %,
c) Renal disease in 8 %,
d) Thyroid diseases in 5%,
e) Heart problems in 2%.
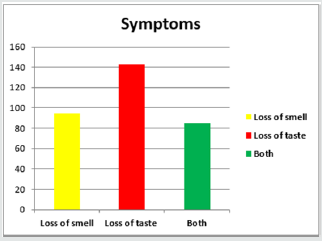
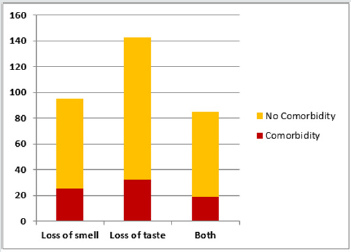
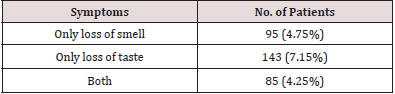
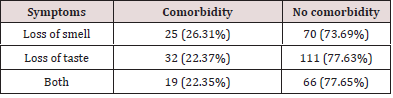
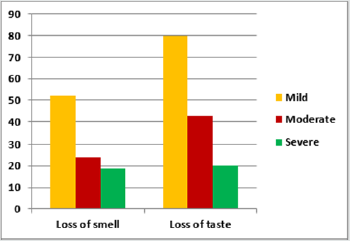
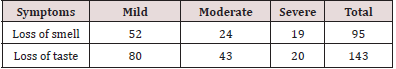
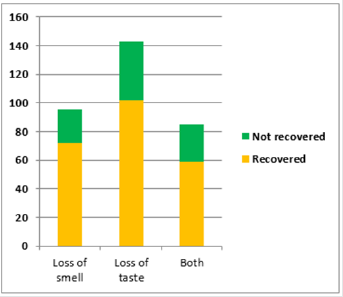
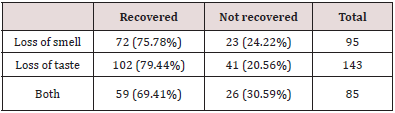
The most common presenting symptom was fever seen in 1500(75%) patients. Other symptoms included cough in 1100 (55%) patients, expectoration seen in 446 (22.3%), breathlessness in 302(15.1%), nausea and vomiting in 80(4%) patients, fatigue/ malaise in 568 (28.4%) patients (Figure 3& Table 3).Other rare symptoms were hemoptysis, chest pain, constipation and diarrhoea. The most common otorhinolaryngological manifestation was sore throat seen in 460 (23%) patients. Other manifestations include running nose in 292 (14.6%), olfactory disturbances in 180 (9%), nasal obstruction in 156(7.8%) patients, headache in 222(11.1%), pharyngeal congestion in 208(10.4%), tonsillar hypertrophy seen in 62(3.1%) patients. Dizziness was seen in 5(0.25%) patients. Epistaxis was seen in 8(0.4%) patients (Figure 4& Table 4).No patients reported facial edema or tenderness, diminution of hearing, hoarseness, or stridor.
Discussion
In December 2019, a novel coronavirus epidemic, caused by the severe acute respiratory syndrome coronavirus–2 (SARS-CoV-2) emerged from China[3]. The disease is widely distributed, making it an important pathogen with an unrestricted health threat [7]. The nasal, nasopharyngeal and/or the oropharyngeal tissue is one of the main harbor sites of the infection, main site of taking the sample for testing and a main source of transmission of infection. However, most published COVID-19 researches are focused on the lower respiratory tract manifestation and sequels due to their life-threatening nature.The literature that is available on ENT manifestation during COVID-19 infection is still sparse, thus, there is value in studying ENT manifestations of such a novel virus[8]. In our study, we have tried to collect the data concerning the ENT manifestations in the laboratory confirmed COVID-19 cases that were mild to moderately symptomatic.In the systematic review conducted by El Anwar M et al. they observed that fever (reported in 73.5% of the included patients), and cough (reported in 61%) are the dominant symptoms ofCOVID-19[8]. The findings of our study were similar with fever being seen in 75% of the patients and cough being seen in 55% of the patients. However, in the study by Salepci E et al, the most common general symptom was fatigue (71.3%) followed by cough (54.3%), and fever (50.7%)[9].
Lovato et al. criticizing the largest meta-analysis study on COVID-19 to date by Sun et al, suggested that true prevalence of sore throat was underestimated[10].In a followup systemic review, Lovato et al. reported that 12.4% of patients had sore throat[11]. In our study, 23% of the patients suffered from sore throat. In the study by Salepci et al, the prevalence of sore throat was 26%[9].In the review by El Anwar et al, the most common ENT manifestations for COVID-19 were sore throat (11.3%) and headache(10.7%).They concluded that their incidence is much less than the incidence of fever and cough in COVID-19 patients[8]. In the study conducted by Sakalli E et al.the most frequent ENT-related symptoms of the patients were nasal obstruction (53.5%), loss of sense of smell (51.2%), sore throat (50.2%), loss of sense of taste (47.1%), and rhinorrhea (38.5%) [12]. In our study the most common otorhinolaryngological manifestation was sore throat seen in 460 (23%) patients. Other manifestations include running nose in 292 (14.6%), nasal obstruction in 156(7.8%) patients, headache in 222(11.1%), pharyngeal congestion in 208(10.4%), tonsillar hypertrophy seen in 62(3.1%) patients. In the review by El Anwar M et al, no emergency ENT symptoms as bleeding per nose or throat or stridor were seen [8]. In our study, 8 patients presented with epistaxis, but there were no cases of stridor or upper airway obstruction.Varia et al.performed objective smell and taste tests were performed on 72 patients with positive PCR for COVID-19 and with no previous history of smell and taste dysfunction.They found that 73.6% of patients had smell or taste dysfunction during the course of the COVID-19 with 14.4% having isolated olfactory dysfunctions [13]. Sakalli Eet al, in their study concluded that loss of sense of smell/ taste is a common symptom in COVID-19 and may be the first and/or only symptom of this disease. In our study, 9% of the patients presented with olfactory disturbance.
In the study conducted by Salepci et al, out of 223 patients, only five patients stated that they had new onset complaints of dizziness and two that of hearing loss[9].They proposed that these complaints might not be related to COVID-19, but simply coincide with disease onset. Auditory manifestation was not reported in the studies on COVID-19 and auditory complication due to coronavirus is little mentioned in the literature[8].In our study, 5(0.25%) patients presented with dizziness, and no patients complained of hearing loss. Otorhinolaryngologic examinations produce aerosol, hence it is important to determine which patients are at higher risk of disease transmission and take the necessary precautions[14,15]. Salepci et al. observed that relying solely on fever measurement and questioning of patients only for general symptoms creates false confidence. They advocated that Otorhinolaryngologist should be alert not only for general symptoms but also for otorhinolaryngologic symptoms that could be associated with COVID-19. The absence of common symptoms must not be interpreted as the absence of the disease[9].
Conclusion
Though, the most common presenting symptoms in COVID-19 patients are fever and cough, a significant proportion of patients does have ENT manifestations which may go unnoticed. Hence it becomes necessary to screen all COVID patients for ENT symptoms so that high quality care can be provided for patients.This also facilitates care givers to take necessary precautions to protect themselves.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/