Lupine Publishers | Journal of Otolaryngology
Abstract
Introduction: The Severe Acute Respiratory Syndrome Coronavirus 2(SARS CoV2), started in Wuhan in China at December 2019.The symptoms mainly included fatigue, fever, dry and productive cough, shortness of breath, chest compression, myalgia, diarrhea, vomiting, anorexia, headache, sore throat, dizziness, palpitations, and, chest pain. Anosmia and/or ageusia may present as a symptom alone in cases of COVID-19. Hence it is necessary to test or quarantine patients with these complaints.
Aims and objectives: To determine the prevalence of anosmia and ageusia in patients with COVID-19 presenting to our tertiary care center.
Materials and Methods: All patients with confirmed real time polymerase chain reaction (RT-PCR) positive testing for the SARS -CoV-2 viral genome was assessed for symptoms and signs of olfactory and taste disturbance.Patients were asked to quantify their loss of sense of smell and taste, subjectively into mild, moderate and severe.
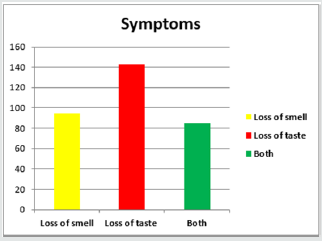
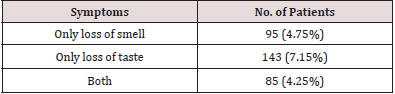
Results: Out of 2000 patients 95 patients (4.75%) had loss of sense of smell, and 143 patients (7.15%) had taste disturbance. 85 patients (4.25%) had both loss of smell and taste sensation. Out of 95 patients with loss of smell sensation, 25 patients (26.31%) had associated comorbidities, 32 patients (22.37%) out of the 143 with loss of taste sensation had comorbidities and 19(22.35%) patients out of the 110 patients with loss of both sensations had associated comorbidities.Out of 95 patients with loss of smell sensation, 72 (75.78%) patients recovered spontaneously. Out of 143 patients with loss of taste, 102 (79.44) patients recovered spontaneously. Among the patients with both symptoms, 59 (69.41%) recovered spontaneously.
Conclusion: Loss of smell and taste sensation is common, especially in COVID-19 disease with mild to moderate symptoms, and it can appear without any other general and ENT-related symptoms associated with COVID-19 disease or it may be the only symptom of COVID-19 disease. During the COVID-19 pandemic, screening tests performed in patients with loss of taste and smell sensation due to suspected COVID-19 disease will allow early diagnosis and treatment of patients.
Keywords: COVID-19; anosmia; ageusia; prevalence
Introduction
The Severe Acute Respiratory Syndrome Coronavirus 2(SARS CoV2) started in Wuhan in China in December 2019[1]. Since then, the new virus, also known as Coronavirus Disease 2019 (COVID-19), has spread dramatically all over the world crossing all borders till the World Health Organization (WHO) confirmed it as a pandemic disease on March 11, 2020 [2].At the initial times of COVID-19 disease, in China, the symptoms mainly included fatigue, fever, dry and productive cough, shortness of breath, chest compression, myalgia, diarrhea, vomiting, anorexia, headache, sore throat, dizziness, palpitations, and, chest pain[3,4].Since then, there has been an increase in studies from different parts of the world about the significant increase in the cases number presenting with loss of smell alone[5].The pathophysiology of loss of smell developing after infection with this virus has been suggested to be due to olfactory epithelial damage or due to spread to the central nervous system[6,7].The behavior of SARS-CoV-2 is different in different patients. This prevents suspicion of the disease clinically, delays diagnosis and isolation of patients infected with the virus, make it difficult to deal with the disease[8].Anosmia and/or ageusia may present as symptom alone in cases of COVID-19. Hence it is necessary to test or a quarantine patient with this complaint. The aim of our study was to determine the prevalence of anosmia and ageusia in patients with COVID-19 presenting to our tertiary care center.
Materials and Methods
All patients with confirmed reverse transcriptase polymerase chain reaction (RT-PCR )-positive testing for the SARS -CoV-2 viral genome were assessed for symptoms and signs of olfactory and taste disturbance. 2000 patients who presented to our tertiary care designated COVID hospital were included in the study. Health workers with confirmed positive PCR test results were voluntarily enrolled in the study. All subjects provided informed consent to participate in the study. Patients were asked to quantify their loss of sense of smell and taste, subjectively into mild, moderate, and severe.
The inclusion criteria were
a) Patients >18 years of age with a positive COVID -19 test.
b) Patients having mild to moderate symptoms.
The exclusion criteria were
a) Age < 18 years old,
b) No confirmed positive PCR test result
c) A history of chronic nasal problems
d) Recent head injury, recent nasal or ear surgery
e) Severe respiratory failure or treatment in the intensive
care unit.
Results
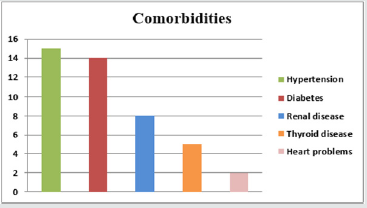
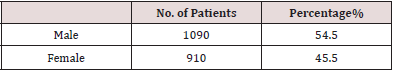
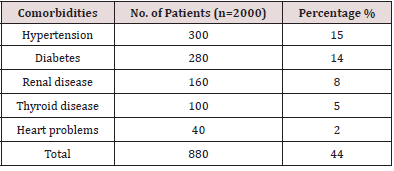
A total of 2000 patients were included in the study. The patients ranged in age from 18 to 70 years, including 1090 males (54.5%) and 910 females (45.5%) (Figure 1& Table 1).The most prevalent comorbidities in these patients were (Figure 2& Table 2).
a) High blood pressure in 15%,
b) Diabetes in 14 %,
c) Renal disease in 8 %,
d) Thyroid diseases in 5%,
e) Heart problems in 2%.
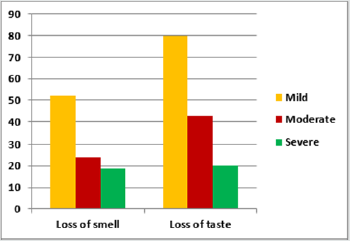
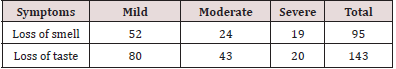
Out of 2000 patients 95 patients (4.75%) had loss of sense of
smell, and 143 patients (7.15%) had taste disturbance. 85 patients
(4.25%) had both loss of smell and taste sensation(Figure 3 &Table
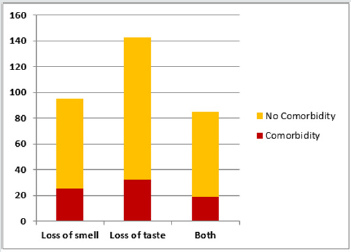
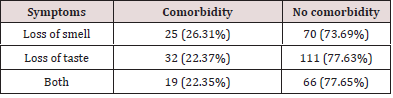
3). Out of 95 patients with loss of smell sensation, 25 patients
(26.31%) had associated comorbidities, 32 patients (22.37%) out
of the 143 with loss of taste sensation had comorbidities and 19
(22.35%) patients out of the 110 patients with loss of both sensations
had associated comorbidities. It can be observed that most
patients with olfactory and taste disturbances did not have comorbidities
(Figure 4& Table 4).Out of 95 patients with loss of smell
sensation, 52 patients (54.73%) had mild loss, 24 (25.27%) patients had moderate loss and 19(20%) patients had severe loss. Out
of 143 patients with loss of taste, 80 (55.94%) patients had mild
loss, 43 (30.06%) patients had moderate loss and 20 (13.98%) patients
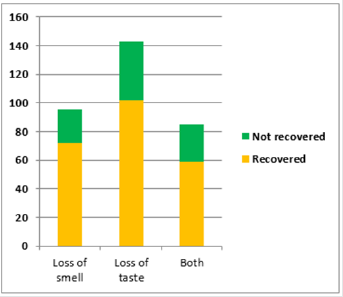
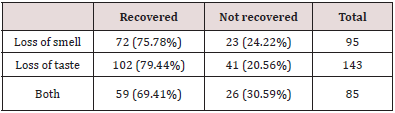
had severe loss(Figure 5& Table 5).Patients were followed up
for 15 days for improvement of symptoms. Out of 95 patients with
loss of smell sensation, 72 (75.78%) patients recovered spontaneously.
Out of 143 patients with loss of taste, 102 (79.44%) patients
recovered spontaneously. Among the patients with both symptoms,
59 (69.41%) recovered spontaneously(Figure 6& Table 6).
Discussion
In December 2019, an epidemic,caused by the severe acute
respiratory syndrome coronavirus 2, emerged from China [9].
COVID-19 can manifest with a wide clinical spectrum that
ranges from no symptoms to septic shock and multi-organs
dysfunction[10].Chemosensory dysfunctions are known to be
common problems during the COVID-19 pandemic [5]. In a study
conducted by Qiu et al, smell and taste abnormalities were the first
and the only complaints in 10% of the subjects, and 25% of the
children had only smell and taste abnormalities at the time of the
presentation [11]. Therefore, these disorders can be considered as
early indicators of COVID-19 disease and is necessary for screening
and control of infection. In our study, we have investigated the
frequency and severity of olfactory and taste related symptoms in
patients with confirmed COVID-19 disease, the association with
coexisting comorbidities,and the recovery process of the smell and
taste disturbances.The first report that included loss of smell and
taste sensation caused by SARS-CoV-2 was of a study conducted
by Mao et al. which emphasized the neurological symptoms of the
disease. They stated that approximately 6% of patients infected
with SARS-CoV-2 had loss of sense of smell and that loss of sense of
smell may be the first symptom before onset of other neurological
symptoms [12]. In the study conducted by Al-Ani R et al, the
prevalence rates of ageusia and anosmia, ageusia, and anosmia
were 8.51%, 11.35%, and 4.96%, respectively [5]. Paderno et al. in
their study observed that the olfactory and gustatory dysfunctions
were seen in 83% and 89% of patients, respectively. Tong et al.
[14] in a systematic review and meta-analysis study [13], observed
that the prevalence rate of the 10 investigations which analyzed
the olfactory dysfunction in patients with COVID-19 disease was
52.73%, whereas nine investigations reported that the prevalence
rate of the gustatory dysfunction was 43.93%.Al-Ani R et al. [15]
postulated that this variability among various studies might be
attributed to the variation in the ethnicity, sample size, and type
of the sample[5].In our study, out of 2000 patients 95 patients
(4.75%) had loss of sense of smell, and 143 patients (7.15%) had
taste disturbance. 85 patients (4.25%) had both loss of smell and
taste sensation.
In a study conducted by Kaye R et al [15], utilizing the COVID-19
Anosmia Reporting Tool developed by the American Academy of
Otolaryngology-Head and Neck Surgery for clinicians indicated
that 73% of 237 patients had loss of sense of smell at admission
to hospital, and 26.6% of these patients had loss of sense of smell
as the main complaint at the time of admission to hospital. They
reported that 85% of the patients who described loss of sense of
smell recovered within the first 10 days, and the average recovery
time was 7.2 days.Lechien JR et al. [16] reported that 67.8% of their
patients with loss of sense of smell and 78.9% of patients with loss
of sense of taste recovered to various degrees within an average
of 8 days [16]. In our study, patients were followed up for 15 days
for improvement of symptoms. We found that 75.78%patients with
loss of smell sensation, 79.44% with loss of taste sensation and
69.4% of patients with both symptoms recovered at 15 days. In a
study conducted by Sakalli E et al, out of 172 patients, 88 patients
were reported to have loss of sense of smell related to SARS-CoV-2
infection. Among them, loss of sense of smell was mild in one
(1.2%) patient, moderate in 24 (14%), and severe in 62 (36.0%)
patients[17]. We found that out of 95 patients with loss of smell
sensation, 52 patients (54.73%) had mild loss, 24 (25.27%) patients
had moderate loss and 19(20%) patients had severe loss. Out of
143 patients with loss of taste, 80 (55.94%) patients had mild loss,
43 (30.06%) patients had moderate loss and 20 (13.98%) patients
had severe loss. It was also observed in our study that most patients
with olfactory and taste disturbances did not have any associated
comorbidities.There are no proven mechanisms for the loss of smell
and taste sensation.There is no prior investigation that studied the
possible association between coronavirus and the appearance of
taste alteration. Zhou et al. [18] have been confirmed that COVID-19
uses the cellular angiotensin-converting enzyme 2[18].It is possible
that the COVID-19 causes taste dysfunction similar to that caused
by the ACE2 inhibitors[19]. Though the mechanisms for the smell
and taste loss in COVID-19 disease are unclear, we observed that
SARS-CoV-2 does cause loss of smell and taste sensation in infected
patients, and that majority of patients recover spontaneously.The
limitations of our study include the following:
a) Subjective assessment was done, and objective diagnostic
tests were not used to evaluate the severity and frequency of
the STL symptoms and improvement of STL.
b) We did not include patients with severe symptoms and
those treated in the intensive care unit. Therefore, our study
population might not be representative of all patients with
COVID-19 disease.
c) Patients were followed up for 15 days for assessment of
recovery of smell and taste sensation, therefore we do not have
long term follow-up results for patients who did not recover
within 15 days.
Conclusion
Loss of smell and taste sensation is common, especially in COVID-19 disease with mild to moderate symptoms, and it can appear without any other general and ENT-related symptoms associated with COVID-19 disease or it may be the only symptom of COVID-19 disease. During the COVID-19 pandemic, screening tests performed in patients with loss of taste and smell sensation due to suspected COVID-19 disease will allow early diagnosis and treatment of patients.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/

No comments:
Post a Comment