Lupine Publishers | Journal of Otolaryngology
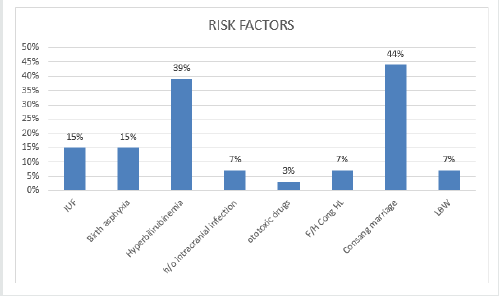
Abstract
Adenoid cystic carcinomas (ACC) of the sinonasal tract is a malignant neoplasm, characterized by slow and insidious growth. Thus, patients usually present in advanced stages. Clinical presentation is unspecific. Treatment is based on surgery followed by radiotherapy. Since the tumor spreads through perineural and hematological routes, delayed metastasis and local recurrence may occur several years after remission. In the present manuscript, we report the case of two patients who present with an ACC of the maxillary sinus diagnosed in an advanced stage. Orbital and cerebral involvement was objectified in one patient. Treatment consists in surgery. Post-operative radiotherapy was performed in one patient. He had a complete remission. Loco-regional recurrence occurred in the second patient. ACC is a particular entity among sinonasal cancers. Further studies are needed to define multimodal treatment including surgery, radiotherapy, and chemotherapy
Keywords: Adenoid cystic carcinoma; sinonasal tract; surgery, radiotherapy
Introduction
Adenoid cystic carcinoma (ACC) of the sinonasal tract is a rare cancer that originates from salivary glands [1]. It is the most frequent malignancy in the maxillary sinus among non-squamous cell carcinomas [2]. Clinically, it presents as a slow growing and locally aggressive tumor with a tendency to local recurrence and late metastasis [3]. Through two cases report, we illustrate clinical, histological, and therapeutic characteristics of sinonasal ACC.
Case Presentation
Case 1:
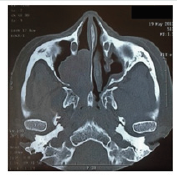
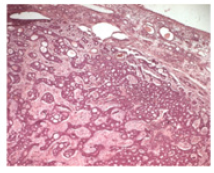
A 50-year-old female patient, with no medical history, presented with right nasal obstruction, epistaxis and nasal discharge that appeared one year ago. Physical examination found a mass of the right nasal cavity. The neck was free from lymph nodes. The neurological and ophthalmological examination were normal. CT scan showed a 5 cm mass, occupying the right maxillary sinus (Figure 1). Tumor extended to the ethmoid and the right nasal cavity. A biopsy of the lesion was performed. Histological examination (Figure 2) concluded to ACC with a cribriform type. No metastasis was found. Tumor was classified T3N0M0. Patient was operated on by Rouge-Denker technique. Post-operative radiotherapy was performed. Patient had regular clinical and radiological follow-up. No recurrence was noted during the 10 year-follow-up.
Case 2:
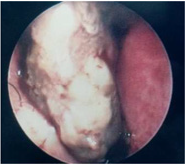
A 39-year-old male patient, presented with unilateral rhino logical symptoms (epistaxis, rhinorrhea, and nasal obstruction) evolving for 5 months. At the physical examination, we found a nasal deformity and a bleeding mass of the left nasal cavity (Figure 3) that extended to the nasopharynx. A left exophthalmia was noted. No cervical lymph nodes were found. The ocular motility and the fundus examination were normal. MRI was performed and showed a mass of the left maxillary sinus which was isointense on both T1 and T2-weighted sequences. Extension to the nasal cavity, nasopharynx and left orbit was objectified. Tumor was removed by paralateronasal approach. Post-operative radiotherapy was planned. Unfortunately, orbital, and cutaneous recurrence occurred. Thus, palliative radiotherapy was achieved.
Discussion and Conclusion
Sinonasal tract malignancies are rare tumors that account for
3% to 5% of all the upper aerodigestive tract cancers [4]. Among
these malignancies, ACC is the most frequent salivary gland cancer.
It represents 10% of all malignancies at this site [5,6] and about 10%
to 25% of all ACCs of the head and neck [7]. It is a slow-growing and
locally aggressive tumor with clinical, biological, and therapeutic
characteristics. Mean age at diagnosis is 55 to 57-year-old [8]. ACC
is thought to be hormonally dependent. A female predominance
was noted in literature [9]. Tumor growth is insidious thus,
patients are asymptomatic for a long period and may present with
advanced-stage disease [3] . ACC is also characterized by a tendency
for perineural spread along major and minor nerves which makes
the treatment challenging [10]. Most frequent signs are nasal
obstruction, epistaxis, nasal discharge, facial pain and dysosmia [6]
likewise our patients. This unspecific presentation leads generally
to a delayed diagnosis. When the tumor reaches large dimensions
and invades surrounding bone and structures, severe signs appear
such as headaches, seizures, ophthalmoplegia, diplopia and
trigeminal neuralgia [6,8]. The occurrence of neurological and
ophthalmological signs is correlated with poor prognosis [3]. The
maxillary sinus is the most common site followed by the nasal cavity
and the ethmoid sinus [8,11]. The frontal and sphenoid sinuses are
correlated with a worse survival rates due to their proximity to the
skull base [7]. Skull base involvement and intracranial extension
are remarkably high. Cervical lymph node metastases are rarely
reported. They accounted for 6% in the series of Rhee [11], 3.6%
in the series of Unsal [7] and none of our patients. Lymph node
involvement is correlated with poor prognosis as they represent a
risk factor for distant metastasis and low survival rate [12].
Histologically, ACC is composed of three subtypes: tubular,
cribriform, and solid [7]. The cribriform subtype is the most
common one whereas the solid subtype has the worst prognosis
[11]. Treatment of sinonasal ACC is based on surgery, followed
by radiotherapy [13]. According to Lupinetti et al., overall, and
disease-specific survival are improved when patients are treated
with surgery and postoperative radiation compared with other
treatment modalities [6]. The aim of surgery is to ensure complete
tumor removal with negative margins. However, surgery of
advanced stages tumor is challenging and can result in serious
morbidity, especially when critical anatomic structures are involved
such as the brain, the orbit, the cranial nerves, and the nasopharynx
[10]. In our series, tumor extended to the nasopharynx and orbit
in one patient. ACC is a radiosensitive tumor but not radio curable
[13]. Postoperative radiotherapy aims to clear positive margins
left after surgery [14]. Long-term survival does not seem to be
improved when radiotherapy is associated, but 5-year diseasefree
period is slightly prolonged [7]. In the study of Rhee, the
5-year local recurrence rate was 42% in T3 and T4 stages despite
postoperative radiotherapy was performed in most of the patients
[11]. Radiation therapy alone is indicated in T4 unresectable tumors
[15]. Chemotherapy has not proven effectiveness in ACC treatment.
Further clinical trials using combined therapeutic approaches are
required [11]. ACC is characterized by local recurrence and distant
metastasis that can occur several years after initial treatment and
remission [11]. In the series of Miller, local failure rate was 50%.
This high rate was explained by the high proportion of patients
diagnosed in advanced stages [10]. In other studies, treatment
failure rates range from 60% to 70% [15]. ACC of sinonasal tract has
a poor prognosis. The most relevant prognosis factors are tumor
site, skull base invasion, stage, histopathologic type, and treatment
modalities. Treatment is based on surgery. Even though ACC is not radio
curable, post-operative radiotherapy improves locoregional
control. Early diagnosis, applying the appropriate therapeutic
approach and long-term follow-up are the mean guarantees to
improve prognosis.
Funding and Conflict of Interest
Authors declare that they have not receive any financial support. No conflict of interest.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/