Abstract
Background: Loss of smell and taste are common complaints in patients with the COVID-19 disease. These symptoms may
present alone or with other symptoms. It is of utmost importance to know their rates of occurrence for better controlling of the
infection.
Objectives: To detect the prevalence of anosmia and ageusia in individuals with COVID-19 in Al-Wajbah Primary Health Center,
Doha, Qatar.
Materials and Methods: This retrospective cohort study was conducted at Al-Wajbah Primary Health Center, Doha, Qatar.
The study covered the two-month period -May and June 2020. The proven cases of COVID-19 by real-time PCR (Polymerase Chain
Reaction) were enrolled in the study. Data regarding the age, gender, symptomatology including anosmia and ageusia, history
of recent travel, smoking, past history of nasal and paranasal diseases (NPND), and severity of the disease were taken from the
patients’ records. IBM- SPSS version 22 statistical software was used for the analysis of the data.
Results: Out of 141, 35 (24.82%) subject presented with
anosmia, ageusia or both. Most of the patients were from age group
>30 year (n=104, 73.76%) with nearly equal gender. The majority of
the individuals were without history of recent travel (92.2%)
and smoking (80.14%). Three-quarters of the patients were asymptomatic,
and 51.06% with a past history of NPND. The male sex,
history of recent travel, smoking, and severe course of the disease were
positive, highly significant association with anosmia or
ageusia. All patients returned to their normal smell and taste
sensations within a mean duration of 6.89 days.
Conclusion: Loss of taste and smell were common symptomatology of COVID-19 disease. The males, recent travel, smoking, and
severe course of the disease were risk factors of the anosmia and ageusia in COVID-19 cases.
Keywords: Anosmia; Ageusia; Prevalence; COVID-19; Qatar
Introduction
On the last day of the year 2019, 41 patients with pneumonia
of unidentified cause were detected in Wuhan City, Hubei province
in China [1]. The identification of the causative microorganism was
reached from the examination of the throat swab samples from
the Chinese Centre for Disease Control and Prevention (CCDC) on
7thJanuary 2020. The causative agent was named Severe Acute
Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). The World
Health Organization (WHO) in February 2020 named the disease
as COVID-19 [2]. During the outbreak of COVID-19 infection, there
were millions of infected people and hundreds of thousands of dead
all over the world, and it remains a global threat [3].The source of
coronavirus was found to be in a “wet market” in Wuhan, China,
where meats from both live and dead animals are sold. The animal source
of coronavirus is still debated, while most officials agree
that the original host of the virus was a bat. Bats have also found
to host other deadly viruses like Ebola, HIV etc. The coronavirus is
a family of viruses that causes diseases in several animals. Seven of
the viruses within this family and the new one has made the jump
across the inter-species barrier and infected human, with most
causing flu-like symptoms.The attention worldwide focused mainly
on the infected cases and those with direct contact with patients.
The asymptomatic carriers were not being tested because of the
shortage in testing kits including all the suspicious cases even in
developed countries with a good health system like the US and the
UK [4]. So, it is of utmost importance to evaluate the number of
predictive symptoms of this disease in order to decide for a
selfisolation
and prevent the spreading of the infection.
At the initial times of COVID-19 disease, the symptoms of the
inpatient cases in China included fatigue, fever, dry and productive
cough, shortness of breath, chest compression, myalgia, diarrhea,
vomiting, anorexia, headache, sore throat, dizziness, palpitations,
and, chest pain [5,6]. After that, there have been an increment in
the scientific studies from various parts of the world about the
significant increase in the cases number presenting with loss of
smell alone. Gilani et al. from Iran reported 8 patients with anosmia,
5 of them were confirmed cases of COVID-19, and the remaining 3
cases were not tested owing to the shortage of testing kits in the
pandemic period [7]. A European multicenter study concluded that
olfactory (85.6%) and gustatory (88%) abnormalities are prevalent
symptoms in European confirmed COVID-19 cases, who may not
have other nasal complaints [8]. However, these cases do not meet
the criteria of self-isolation or testing [9].Anosmia and/or ageusia
might present alone or in mild confirmed cases of COVID-19. It is
therefore necessary to test or quarantine those individuals with
these complaints.We aimed to determine the prevalence of anosmia
and ageusia in patients with COVID-19 in Al-Wajbah Primary Health
Center, Doha, Qatar.
Materials and Methods
This retrospective cohort study was conducted at Al-Wajbah
Primary Health Center, Doha, Qatar during May, and June 2020.
Patients with proven COVID-19 infection by real-time PCR on
nasopharyngeal and oropharyngeal swabs were enrolled in the
current study. The PCR swabs were tested at the pathological
laboratory of Hamad Medical Corporation, Qatar for the corona
virus using the Abbot m2000 Real Time device patented in South
Africa. Subjects with incomplete data, previous anosmia or ageusia,
psychological disturbances, and those who lost to follow-up (not
responding to 3 telephone calls) were excluded from the study. We
had 180 covid-19 positive patients during our study period, out
of which only 141 patients were included in this study.ICleanhcy
Specimen Collection Flocked nylon swabs-Huachenyang (HCY)
made in USA was used to collect the samples from all the individuals
Data regarding the age, gender, history of recent travel, presenting
symptoms (fever, myalgia, cough, dyspnea, fatigability, sore throat,
anosmia, ageusia, diarrhea, etc.), past nasal and paranasal diseases
(NPND), history of smoking, and the severity of the disease were
taken from every patient who tested positive. The patients were
divided into asymptomatic and symptomatic. The severity of the
symptomatic diseases was classified into [10]:
a) Mild patients complained from only low-grade fever, mild
cough, and slight fatigue.
b) Moderate patients complained from high grade fever and
moderate respiratory symptoms. Findings of pneumonitis were
seen in chest radiograph.
c) Severe patients had dyspnea, respiratory rate 30/min,
blood oxygen saturation 93%, partial pressure of arterial
oxygen to fraction of inspired oxygen ratio 300 mm Hg, or CT
scans showing at least a 50% increase in infiltrate volume over
24-48 hours.
d) Critical patients had respiratory failure, septic shock,
and/or multiple-organ dysfunction or failure.
IBM-SPSS statistical software version 22 was used for analyzing
the data. Chi-Square test was used to compare between categorially
variables. One sample T-test was used for the comparison of the
means. P-value was considered a statistically significant difference
if it is less than 0.05.
Results
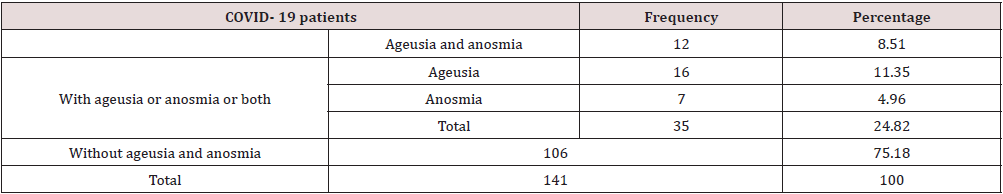
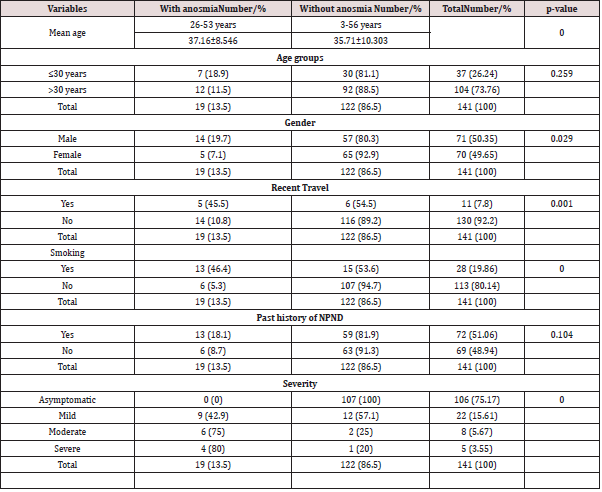
Out of 180, 141 patients fulfilled the inclusion and exclusion
criteria, were thus enrolled in the study. The prevalence rates of
ageusia and anosmia, ageusia, and anosmia were 8.51%, 11.35%,
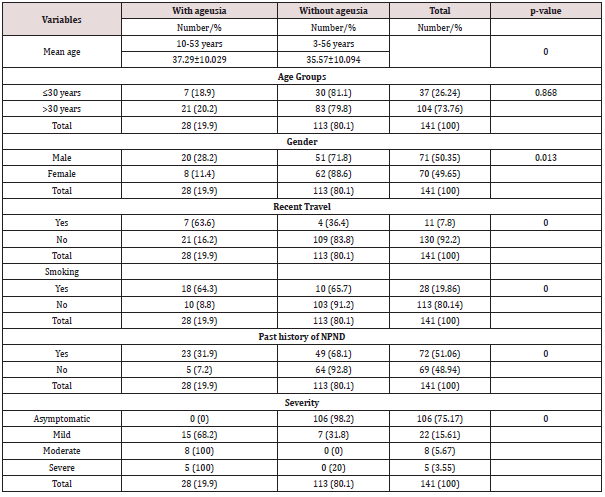
and 4.96 respectively as shown in Table 1. The age of the patients
ranged from 3-56 years with a mean age of 35.91year±10.069.
The age range of the patients without anosmia 3-56 years was
wider than those with anosmia 26-53 years, and there was a high
statistically significant difference between the mean ages of both
groups (p-value=0.000) Table 2. The highest age group affected by
COVID-19 disease was >30 years (n=104, 73.76%). The males 71
(50.35%) was slightly more than females 70 (49.65%). Most of our
patients were without history of recent travel 130 (92.2%). The
majority of the cases were without history of smoking (80.14%).
Three-quarters of the cases were asymptomatic as shown in Tables
2 & 3. There was a positively statistically significant difference
between the 2 groups of patients (with and without anosmia)
regarding the following factors the male sex, history of recent
travel, smokers, and severe course of the disease. While, there
was no statistically significant difference between both groups
regarding the age group and past history of NPND (p-value>0.05)
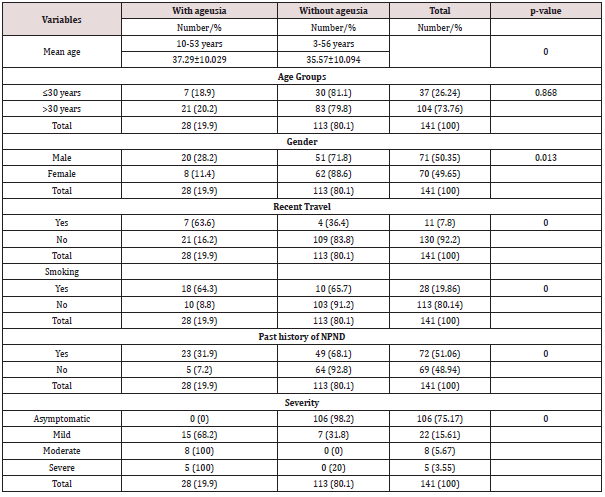
as shown in Table 2. The age ranged of the subjects without ageusia
3-56 years was wider than those with ageusia 10-53 years, and there was a high statistically significant difference between the
mean ages of both groups (p-value=0.000) Table 3. There was a
positively statistically significant difference between the 2 groups
of patients (with and without ageusia) regarding the following
factors the male sex, history of recent travel, smokers, past history
of NPND, and severe course of the disease. While, there was no
statistically significant difference between both groups regarding
the age groups of the patients (p-value>0.05) as shown in Table
3. All patients were showed full recovery from the anosmia and
ageusia with a resolution time of 3-12 days with a mean of 6.89
days±3.056. No death was reported in our study.The following
tables show the variability indices of the symptoms of the covid-19
infected patients
Table 1: The distribution of 141 patients with COVID-19 disease.
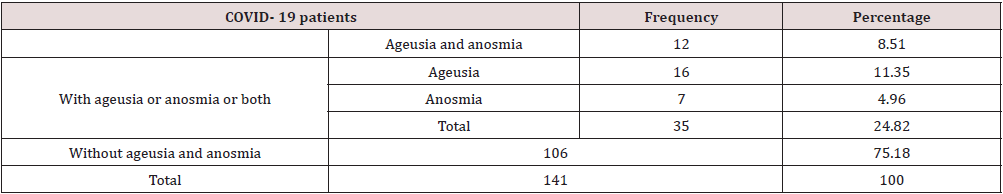
Table 2: The relationship between socio-clinical characteristics and anosmia of 141 patients with COVID-19.
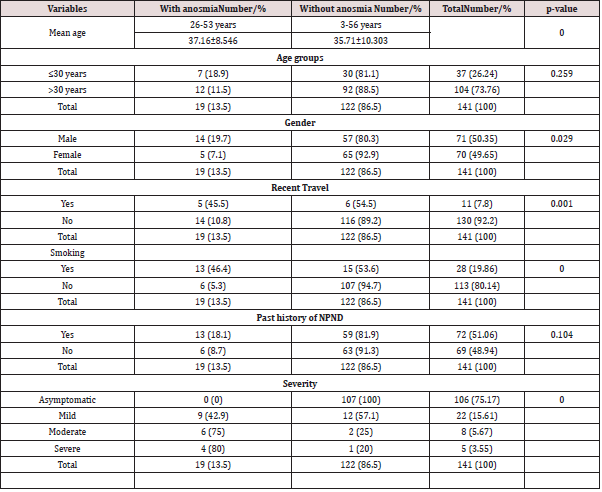
Table 3: The relationship between socio-clinical characteristics and ageusia of 141 patients with COVID-19.
Discussion
Chemosensory dysfunctions are common problems during the
pandemic COVID-19 crisis. Smell and taste Abnormalities (STA)
were the first and the only complaints in 10% of subjects, 19%
experienced STA before other classical symptoms like fever and
cough, as well as 25% of the children had only STA at the time of
the presentation [10]. Therefore, these disorders are indicators of
early cases of COVID-19 disease and necessary for screening and
infection control. Our study design included a questionnaire for
patients about anosmia, ageusia, or both only to overcome the bias
due to unrecognized pre-existing chemosensory hypo-function, and
the difficulties in catching these hypo-functions as they are highly
subjected to personal variation in response to the questioner, and
the stressful conditions of the patients. The prevalence rates of
ageusia and anosmia, ageusia, and anosmia were 8.51%, 11.35%,
and 4.96%, respectively, making the overall prevalence rate 24.82%
Table 1. Qiu et al. multi-centric case series study found that 41%
of the COVID-19 patients complained from STA [10]. Speth et al.
reported that the prevalence rate of olfactory dysfunction was
61.2% [11]. Paderno et al. showed that the olfactory and gustatory
dysfunctions were seen in 83% and 89% of patients, respectively
[12]. In a systematic review and meta-analysis study by Tong et
al. found that the prevalence rate of the 10 investigations which
analyzed the olfactory dysfunction in patients with COVID-19
disease was 52.73%. While nine investigations reported that the
prevalence rate of the gustatory dysfunction was 43.93% [13].
The study by Chary et al. found that the rate of STA without nasal
complaints was 70% [14]. The variability among various studies
might be attributed to the variation in the ethnicity, sample size, and
type of the sample (children or adults or both, hospitalized,
nonhospitalized
or both, with or without nasal symptoms, subjective,
objective or both assessment, and severity of the disease).There are no
proved mechanisms for the STA. There is no prior investigation
that studied the possible association between coronavirus and the
appearance of taste alteration [15].
The study by Zhou et al. have been confirmed that COVID-19 uses
the same receptor [cellular angiotensin-converting enzyme 2 (ACE
2)] as SARS-CoV[16]. The enzyme found in the mouth, particularly
on the tongue. Therefore, it is possible that the COVID-19 causes
taste dysfunction same as the ACE2 inhibitors [17]. Secondly, the
taste disturbance in the presence of smell abnormality is that both
chemosensory senses are intimately correlated [18]. The study by
Brann et al. [19] suggested that the COVID-19 virus affects the nonneuronal
olfactory epithelium causing anosmia and the associated
taste dysfunctions. This is the most acceptable mechanism because
most of the patients with COVID-19 infection are of the mild
severity, outpatient cases, and most of the STA resolve within short
period [8,20]. However, a large number of a cohort investigation
with long term follow-up and objective measures of the assessment
are needed to assess the exact time and rate of recovery of the STA
in confirmed cases of COVID-19 infection.In a study by Vaira et al.
[21] found that 66% of patients reported spontaneous resolution
of STA on subjective self-reported questionnaire. While, 80%
of these individuals were still revealed a slight disturbance in
their chemosensory functions on objective evaluation measures.
The authors revealed two possible causes for this observation.
Firstly, the patients might be suffering from preexisting unnoticed
chemosensory dysfunctions and secondly, the patients might
consider the great improvement in these senses as normal. The
present study was used the self-reported questionnaire on the
evaluation of the anosmia or ageusia resolution in COVID-19
cases. Fortunately, all patients showed resolution with a mean of
6.89 days. This finding was higher than what was reported in the
prior investigations [8,21]. However, self-reported evaluation was
a shortcoming of the present study. we recommend a further study
to use objective assessment of these chemosensory alterations in
COVID-19 cases.
The study found that there was an equal gender distribution,
but males with anosmia and ageusia were more prevalent than
females (p-value<0.05). This finding was in contrast to the prior
studies [8,10-12,14,21,22]. This difference between our study and
the previous studies might be attributed to the differences in the
social and cultural behaviors and geographical locations. Many
investigations reported that younger patients had a positive impact
on the resolution of the STA [11,14,21]. Despite, approximately 75
% of the patients were more than 30 years, our study found that
the age was not considered a significant factor in relation with a
resolution of anosmia and ageusia (p-value>0.05). Similar finding
was reported by the previous study [12].In the early period of
COVID-19 disease, recent travel is considered as an important factor
for the transmission of the disease. But as the time progresses and the
infection becomes a worldwide disease, recent travel becomes
less important. Moreover, the contact with suspicious or proved
COVID-19 cases is an important way of the transmission of the
infection to healthy people. Our findings revealed that recent travel
had a significant factor for those patients with anosmia, ageusia or
both (p-value<0.05). However, the study did not find a cause for this
difference. Smoking has adverse effects on the health state of the
lungs and the human immune system. Therefore, smokers are more
vulnerable to acquire infectious conditions. Previous investigations
showed that the smokers are twice more infected with influenza
than non-smokers as well as they are associated with a more severe
course of illness. Besides, there were more deaths among smokers
than the non-smoker during the MERS-CoV outbreak [23]. Moreover,
smoking has a negative impact factor on the severity and clinical
outcome in patients with the COVID-19 disease [23]. However, our
study reported low prevalence of smokers (20%) in patients with
the COVID-19 disease. This finding was similar to Speth et al. study
[11] who they reported that 8.8% of their patients were current
smokers. The current study and Speth et al. studies didn’t find an
explanation of this contradiction. Despite, the low prevalence of
smokers in the present study, the smoking was a highly statistically
significant association with anosmia and ageusia (p-value=0.0000).
It is obvious that the nasal and paranasal problems like nasal
polyposis have a drawback on the smell because they interfere with
air current from reaching the olfactory epithelium in the roof of the
nose. Besides, they might give some sort of taste hypofunction. The
study by Paderno et al. [12] reported that nasal congestion is a risk
factor for late recovery of the STA in the COVID-19 cases. Speth et al.
[11] found that patients with this disease had also allergic rhinitis
(35%), chronic rhinosinusitis (1%), and asthma (12.6%). Although,
half of our cases gave NPNDs, but they were not considering a
significant association with anosmia (p-value=0.104). The highly
significant association between the NPNDs and ageusia was found
in our study. Therefore, it is logical to ask in the history about these
problems when one wants to manage a case of the STA. Olfactory
dysfunction is generally a first symptom in COVID-19 disease
[8,11,23]. The study by Yan et al. [24] reported that the mild disease
had a statistically significant association with the STA. Severe disease
type is usually not associated with the STA. Therefore, the STA can
act as a major positive factor for the prognosis of Covid-19 disease.
However, this theory is of limited in actual clinical practice because
the hospitalized patients in the critical care unit are not able to give
interview due to their bad health condition [14]. Fortunately, there
was no patient in our study needed admission to the intensive care
unit. The current study found a statistically significant association
between anosmia and ageusia and severe disease type. This finding
was in contrast with Yan et al.[20]. This may be attributed to the
difference in the inclusion criteria (anosmia and ageusia in our
study versus STA in Yan et al. s study). The limitations of the study
included small sample size, did not register the time of onset of
anosmia and ageusia, and the study was not used for objective
measures of assessment.
Conclusion
The prevalence of anosmia and ageusia was 24.82%. They
occur mostly in the age group >30 years with equal sex distribution.
Most patients without history of smoking and recent travel. Half of
the patients gave a past history of NPNDs. The majority of the cases
were asymptomatic. The male sex, recent travel, smoking, severe
type of the disease was considered risk factors of the anosmia and
ageusia. Resolution of these symptoms occurred in 100% of the
involved patients with a mean resolution time of 6.89 days.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/