Lupine Publishers | Journal of Otolaryngology

Eagle’s syndrome was a rare condition, and it was not commonly
suspected in clinical practice. The elongation of the styloid
process (SP) was considered as the main cause of this syndrome. However,
many patients who were incidentally found of an
elongated SP were asymptomatic. This case report presented a rare case
of the bilateral elongated SP with the unilateral symptom.
A 59-year-old woman who had come to our attention with the complaint of
pain in the right side of the neck, and intensified pain
during neck rotation, swallowing and mouth opening. She also complained
of pain in the angle of the mandible, the face and otalgia.
The computed tomography scans and 3D reconstruction allow us to measure
the angulation and length of the SP as well as evaluate
the relationship between the SP and adjacent anatomical structures.
Surgical excision was performed on the right side although the
patient was diagnosed with bilateral elongated SP. The postoperative
course passed regularly, and the postsurgical control showed
no complaint.
Keywords: Eagle’s Syndrome; elongated styloid process; stylohyoid complex
Introduction
The styloid process (SP) is a projection of thin, cylindrical and
along bone from the temporal bone, and its location is between the
internal and external carotid artery. The mastoid process and the
tonsillar fossa are at the posterior and inside it, respectively [1].
The styloid process is one part of the stylohyoid complex including
stylohyoid ligament, lesser horn of hyoid bone [2]. Initially,
elongated SP syndrome or Eagle’s syndrome was described by an
otorhinolaryngologists, Dr. Watt Eagle [3]. The symptoms have
diversely presented with ipsilateral cervicofacial pain, referred
otalgia, sore throat, dysphasia, headache, and a foreign body
sensation in the pharynx. The pain regularly limits in the angle of
the mandible, and neck mobility will be reduced when the head
rotates to the affected side [1,4]. A physical examination is induced
by digital palpation of elongated SP through the tonsillar fossa,
and once palpated, the symptoms may intensify. The diagnosis is
often misleading because of the vagueness of symptoms as well
as the infrequent clinical observation, and these patients seek a
variety of treatments in several different clinics such as dentistry,
neurosurgery, neurology, psychiatry. These treatments do not
relieve the symptoms, and they make the whole clinical picture
cloud [4,5]. The mean length of the styloid process ranged from 20
to 25 mm [6,7]. Generally, the SP is considered elongation when it
is beyond 30 mm [6,8]. There are two types of this syndrome: the
classic and the carotid artery type. The former type, also known
as stylalgia, always following tonsillectomy, and usually related to
the elongated SP. The latter type is characterized by nonspecific
symptoms that are caused by compression of the sympathetic
fibers and carotid arteries, and the most common etiology of the
syndrome that is the mineralization of the stylohyoid ligament [7,9].
Eagle’s syndrome is caused by an elongated SP, on the contrary,
the presence of an abnormal length of SP does not result in Eagle
syndrome. Here, we present a case with unilateral Eagle syndrome
and bilateral elongation of the SP
Case Report
A 59-year-old woman presented to the Department of
Otorhinolaryngology, Khanh Hoa general hospital, Viet Nam with
the complaint of pain in the right side of the neck, the angle of the
mandible, the face and otalgia that had started approximately one
month previously. She simultaneously complained of intensified
pain during neck rotation to the right side, swallowing and mouth
opening. The patient was uneventful for any surgical or trauma
history. In the physical examination, the pain was felt when
palpation was performed at the angle of mandible, sternomastoid
muscles. Intraoral examination, the SP was not felt on palpation of
the tonsillar fossa. No particular abnormalities were detected in
the video-laryngoscopic examination and neck ultrasound. Finally,
the symptoms did not improve following medical therapy. Thus,
the patient underwent a CT scan with the 3D reconstruction of the
head and neck (Figure 1). The CT examination revealed a bilateral
elongation of the SPs. The SPs were measured 36 mm on the right
side and 38 mm on the left side (Figure 2). Lidocaine (2%) was
deeply infiltrated into the lateral tonsillar fossa on the right side.
After infiltration, immediate relief of the pain partially supported
the diagnosis of Eagle’s syndrome. Although the SP on the left side
was longer than another on the right side, we decided to do a right
styloidectomy because of no symptom revealing on the left side.
The styloidectomy was made via the intraoral surgical approach
(Figure 3). Antibiotic was administered preoperatively. The surgery
was under general anesthesia and the postoperative period passed
regularly. The patient was discharged on the second postoperative
day. At regular postoperative examinations, complete remission of
symptoms was accomplished.
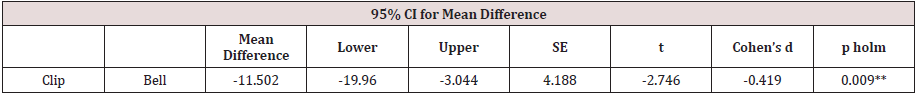
Figure 1: Computed tomography scan with 3D reconstruction on the left (A) and right (B) side that showed an elongation of
the SPs (orange arrows).
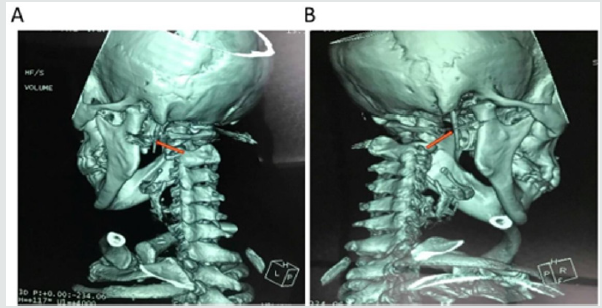
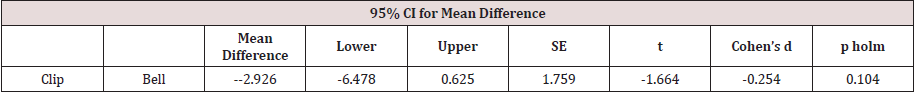
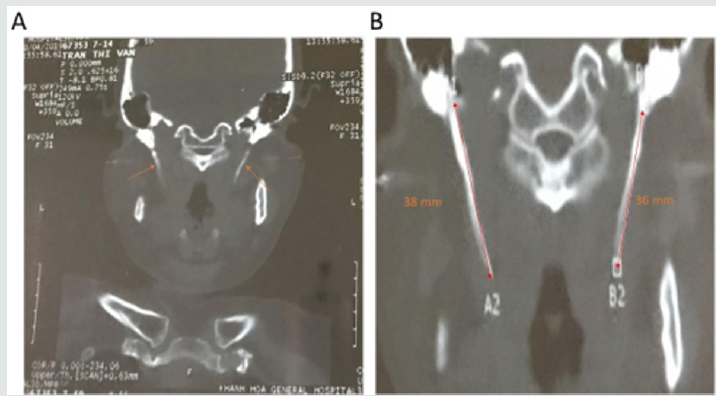
Figure 2: A 59-year-old woman reported neck pain on right side of the face during neck rotation to right side and while
swallowing and opening her mouth. CT examination showed the bilateral elongation of the SPs (A), which was long elongated
on the left than on the right side (B). The SPs measured 38 and 36 mm on the left and right side, respectively (B).
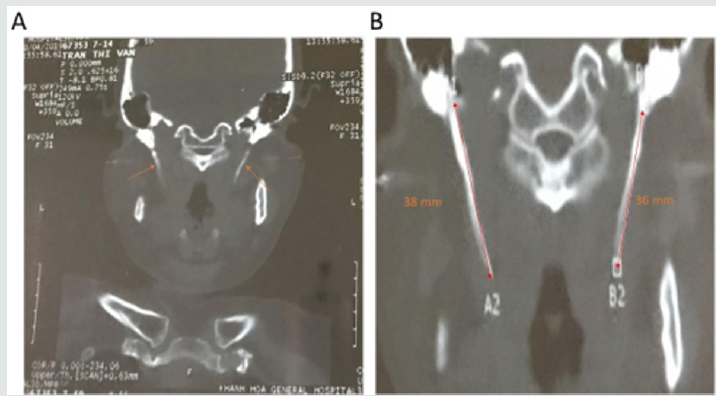
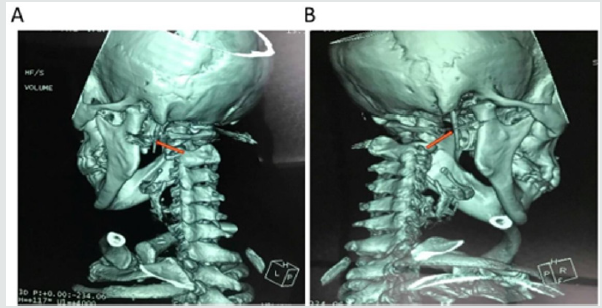
Figure 3: Intraoral approach to the styloid process.
Tonsillectomy was performed first on the right side. The palpation of
the
tonsillar bed was performed, and the tip of the right SP was identified.
The mucosa was dissected longitudinally at the point of
the felt tip in the tonsillar fossa. To avoid vascular injury, the
parapharyngeal space was carefully dissected by q-tips. Palpation
was occasionally performed during surgery to identify the location of
the SP. After the SP was exposure and excised, the
tonsillar bed was carefully sutured with absorbable sutures.

Discussion
The stylohyoid complex (SC) was formed by the SP, stylohyoid
ligament, lesser cornea of the hyoid and superior portion of the
hyoid corpus. Embryologically, these have been derived from
Reicher’s cartilage (the second branchial arch) [6,10]. Based on
the successive development of the SC, it could be divided into four
sections. The most proximal SC was known as the tympanohyaland
which gave rise to the tympanic portion of the SP. The second
portion, known as the stylohyal, forming the distal portion of the SP.
The third portion (the ceratohyal) degenerated in utero, and it gave
rise to the stylohyoid ligament. The most distal portion, known as
the hypohyal, forming the lesser cornu of the hyoid bone [10]. The
SP originated from the temporal bone behind the mastoid, and it
ran anteromedially. Its anatomical variation was rarely changed in
course, and it passed between the external and internal branches
of the carotid artery. Cranial nerves including n. accessory, n.
hypoglossus, n. vagus and n. glossopharingeus were placed
medially to the SP. Three muscles (stylopharyngeus, stylohyoid and
styloglossus) and two ligaments (stylohyoid and stylomandibular)
were attached on the SP [2,5,10]. The length of the SP was individually
variable, and the SP was considered as the elongation whenever it
was longer than 30 mm. However, the existence of an elongated
SP was not pathognomonic for Eagle’s syndrome, because many
patients who were found of an elongated SP were asymptomatic
[10]. Moreover, the elongation of the SP occurred in approximately
4% of the population [11], and only 4% of this group complained
of symptoms [1,12]. Several pathophysiological mechanisms were
used to explain the symptoms of Eagle’s symptoms:
a) The proliferation of granulation tissue after traumatic
fracture of the SP induced the pressure on the surrounding
structure [13,14].
b) Compression of adjacent nerves such as the
glossopharyngeal nerve, the trigeminal nerve and the chorda
tympani nerve [1].
c) Insertion tendonitis was known as a degenerative and
inflammatory change which occurred in the tendinous portion
of the connected area of the stylohyoid ligament [1,14].
d) The formation of granular tissue after tonsillectomy or the
direct compression resulted in the irritation of the pharyngeal
mucosa (involvement of the 5, 8, 9, and 10 cranial nerves) [1].
e) The impingement of the sympathetic nerve in the arterial
sheath [15].
Treatment of Eagle’s syndrome was both conservative and
surgical. The conservative treatment included nonsteroidal
or steroidal anti-inflammatory drugs, antidepressants,
anticonvulsants and exercises for the neck [1,7]. The surgical
method involved amputating or removing the elongated SP via the
intraoral or extraoral approach. Both approaches have been known
to have pros and cons in use. The intraoral technique was simpler
and took less time as well as avoided the surgical scar; however,
its disadvantages were injury of the blood vessels, infection of
deep neck spaces and poor visualization of the surgical field. On
the other hand, the extraoral technique through cervical incision
allowed better visualization of the operative field. This technique,
nevertheless, took a longer time, and it could cause injury of the
facial nerve. Moreover, the patient postoperatively recovery was
longer and resulted in a visible scar [16-18]. Routinely, we took
the intraoral approach to our patients. Due to being familiar with
the technique, we have not encountered any of the complications
which were mentioned above. Also, the injury of vascular and
neural tissues was minimal by this method.
Conclusion
The case verifies the possibility that unilateral symptoms
can occur in the bilateral elongation of the styloid process. To
avoid excessive resection, the side of the styloid process should
be selected by the accurate history of the patient, the tonsillar
palpation and radiologic confirmation.
Conflicts of interest
Authors have none to declare
Acknowledgment
This research was supported by Basic Science Research
Program through the National Research Foundation of Korea (NRF)
funded by the Ministry of Education (2018R1A6A1A03025523).
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/