Lupine Publishers | Journal of Otolaryngology
Short Communication
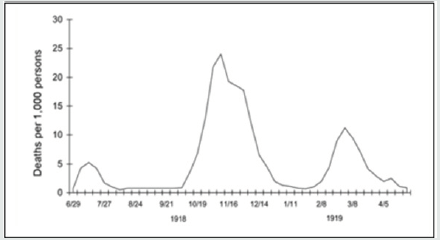
CHistory does not repeat itself. Though every single historical
moment is distinct, parallels can be drawn between different historical
events. Even though history does not teach us what to do, it can inspire
us to act. Revising the 1918 influenza pandemic is an opportunity to
consider the current coronavirus (COVID-19) crisis from a different
perspective. Influenza and coronavirus share basic similarities in the
way they are transmitted via respiratory droplets and contact surfaces.
Descriptions of H1N1 influenza patients in 1918-19 resemble the
respiratory failure of COVID-19 sufferers a century later. Current
discussions about holding back social distancing measures and opening
the country frequently refer to “waves” of disease that characterized
the dramatic mortality of H1N1 influenza in three major peaks in
1918-19. As COVID-19 rates begin to stabilize in some parts of the U.S.,
people today are nervously eyeing the “second wave” of influenza that
came in autumn 1918, that pandemic’s deadliest period.The 1918 influenza
pandemic took place during the First World War with three successive
waves: the first in the spring of 1918, the second – and most lethal,
responsible for 90% of deaths – in the autumn of 1918, and a final one
from the winter of 1918 to the spring of 1919. By the end of it, more
than half of the world’s population had been infected. Estimations on
mortality, showed a broad spectrum ranging from 2.5 to 5% of the world’s
population, which translates to between 50 and 100 million deaths. The
pandemic was, therefore, five to ten times deadlier than the First World
War.
Waves evoke predictability, however, and COVID-19 has been hard to
predict. Despite the lessons drawn from past influenza outbreaks, how
pandemic influenza struck in 1918 is not an exact template for what can
happen with COVID-19 in the upcoming months [1].The 2020 coronavirus and
1918 Spanish influenza pandemics share many similarities, but they also
diverge on some points. Here we empathize some of those points.
According
to Deutsche Bank, a major difference between Spanish flu and COVID-19 is
the age distribution of fatalities. For COVID-19, the elderly has been
hit the worst. For the Spanish flu of 1918, the younger population were
severely affected. The death rate from pneumonia and influenza that year
among the middle-aged population in the United States was more than 50%
higher than that for the older population. Back to COVID-19, the
overall mortality rate measured by weekly new deaths and weekly new
cases is around one-third of the level observed in the second half of
April which shows a decline in the current wave [2].Over 500 million
people, or one-third of the world’s population, became infected with the
1918 Spanish flu. According to the Centers for Disease Control and
Prevention, approximately 50 million people died worldwide, with about
675,000 deaths occurring in the US. They added that during the pandemic,
mortality was high in three categories of people: younger than 5 years
old, 20-40 years old, and 65 years and older. The high mortality in
healthy people, including those in the 20-40-year age group, was a
unique feature of this pandemic. With no vaccine to protect against it
and no antibiotics to treat secondary bacterial infections that can be
associated with it, controlling the disease worldwide were limited to
non-pharmaceutical interventions.COVID-19, the disease caused by the
virus SARS-CoV-2, has already proved extremely infectious. According to
Johns Hopkins University’s Center for Systems Science and Engineering,
it had approximately infected 13.1 million people globally and more than
3.4 million in the U.S. The disease had killed at least 573,664 lives
worldwide and 135,615 in the U.S.As for Symptomatology, for both
COVID-19 and flu, one day or more can pass between a person becoming
infected and when he or she starts to experience illness symptoms.
However, if a person has COVID-19, it usually takes longer to develop
symptoms than if they had flu. For the flu, a person develops symptoms
anywhere from 1 to 4 days after infection but for COVID-19, symptoms can
appear as early as 2 days after infection or as late as 14 days after
infection,
and the time range can vary [3].
Being firstly identified in the Chinese city of Wuhan, some have labeled COVID-19 the ‘Chinese virus’. Stigmatizing a group or a nation for its alleged responsibility in a calamity is not a new trend. Take the misnomer of the ‘Spanish Flu’: unlike most of the countries at war at the time, where censorship was extreme and newspapers were initially not allowed to report on the disease, the Spanish press firstly covered the spread of the virus, creating false assumptions that the epidemic originated in Spain.Many other nicknames were given to the pandemic based on nationality or race, for example: ‘Spanish Lady’, ‘French Flu’, ‘Naples Soldier’, ‘War Plague’, ‘Black Man’s Disease’, ‘German Plague’, or even the ‘Turco-Germanic bacterium criminal enterprise’.War censorship and propaganda also had adverse effects on efforts to mitigate the pandemic. By attempting to censor information on the seriousness of the situation, many belligerent countries most certainly hindered public health efforts to stem the pandemic. Many people did not understand how the flu, an ordinarily mild illness, could cause so many deaths. Some believed their government was lying and trying to hide the return of typhus, cholera, or a so-called ‘pneumonic plague’. In Germany, some people accused the government of using a fake pathogen as a pretext to hide the deaths that were caused by malnutrition and exhaustion according to them.The lives lost during that old pandemic teach us that transparent information is essential at all times(Figure 1). To follow public health measures, the population needs to trust the authorities. In 1918, after four years of conflict and propaganda, that trust was broken. This is even more true in 2020. Mistrust of information from health authorities is still a challenge. Modern means of communication and the digital social networks make it even harder. Undocumented claims, false information, conspiracy theories, and dangerous conclusions can spread as quickly as viruses [4,5].
Figure 1: Three waves of death during the pandemic: weekly combined influenza and pneumonia mortality, United Kingdom, 1918–1919. The waves were broadly the same globally[5].
Conflict of Interest
None declared.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/

No comments:
Post a Comment