Friday, October 30, 2020
Lupine Publishers: Lupine Publishers | Ear, Nose and Throat Disorders...
Lupine Publishers: Lupine Publishers | Onion (Allium cepa) Production...
Lupine Publishers | Normal Oropharynx. An Overlooked Obstruction
Lupine Publishers | Journal of Otolaryngology
Introduction
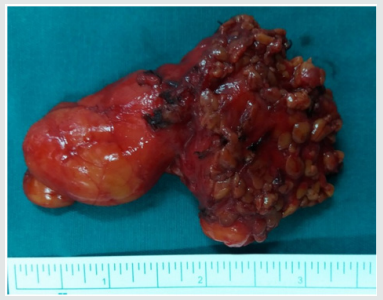
A 35-year-old gentleman with underlying depression presented with noisy breathing and difficulty in breathing and was brought to emergency department by one of his family members. On examination, he was cyanosed and aphonia and an attempt of intubation was tried by an experienced anesthetist but failed. There was ‘no airway’ noticed except for pooling of secretions. The insertion of laryngeal mask airway also failed as there was resistance at the level of oropharynx. In view of rapid desaturation, cricothyroidotomy was performed to secure his airway. Computed tomography of the neck showed an expanded oropharynx (Figure 1). Examination under anesthesia revealed a huge plastic ball swallowed by the patient (Figure 2). It was removed and the cricothyroidotomy was converted to orotracheal intubation. Then he was successfully extubated the next day.
Diagnosis
Oropharyngeal translucent foreign body (plastic ball). Airway foreign body is uncommon in healthy young adults. There is a broad range of presentation from subtle to acute life-threatening airway obstruction. One large-city series of ambulance- transported airway foreign body patients reports a 3.3% mortality (an average of one patient per month) in the prehospital phase alone [1]. History of ingestion of foreign body, inability to swallow and odynophagia are the most important diagnostic criteria [2]. However, it could be challenging among those mentally challenged patients where the history is usually unclear [3]. Therefore, emergency physicians must have high suspicion for foreign body impaction in mind in dealing with this group of patients who present with airway issues. Experienced anesthetist, otolaryngologist must be called in immediately to help out in this kind of difficult airway scenario. In our case, there was a totally occluded airway as the plastic toy ball stuck in oropharynx till cricothyroidotomy was needed. Imaging is usually a useful tool to help locate and delineate the foreign body, but it might be missed in unexperienced hands.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/
Wednesday, October 28, 2020
Lupine Publishers: Lupine Publishers | Onion (Allium cepa) Production...
Friday, October 23, 2020
Lupine Publishers | Hearing Loss A Triggering Factor to Depression: A Systematic Review
Lupine Publishers | Journal of Otolaryngology
Abstract
Introduction: Hearing loss is a hidden disability that affects the hearing ability of an individual and makes it difficult to recognize or discriminate the various auditory signals. People who usually suffer from hearing loss tend to exhibit heterogeneous characteristics comprising of diverse and complex psychosocial behaviours which includes resentment, hostility, rejection and subtle denial resulting to a significant deterioration on socio-emotional development which could ultimately lead to serious mental illness like depression.
Objective: Present review study was conducted to assess the comprehensiveness and trend of various other studies related to impact of hearing loss in individuals leading to depression by assembling diversified online data bases from various sources.
Methods: To conduct this systematic review, a thorough search was framed across multiple databases which was based upon exploration of five facets (“hard of hearing”, “stress and symptoms of depression”, “depression”, “hearing impairment” and “deaf” and). Almost five electronic databases, key texts and references in the articles were identified and critically analysis was done for those articles that had information regarding “hearing loss” and “depression”.
Results: Data accumulated from the databases indicated that hearing loss is a leading factor to depression which has a strong association with the onset and degrees of hearing loss, that acts as a major correlate of depressive symptoms among the geriatric population.
Conclusion: Studies show that there is a considerable propensity for depression among individuals with hearing loss which can also induce suicidal thoughts. Therefore, there should always be an interdisciplinary team approach to establish a well- defined intervention plan for individuals who suffer from hearing loss resulting in mental illness.
Keywords: Hearing loss; Depression; Mental illness
Introduction
Mental health is a condition that has an intensive impact on the general wellbeing of an individual as a whole. It actually acts as reflection which provides a sense of satisfaction to an individual or to the society. In other words, it predetermines how an individual respond to societal issues, inter and intrapersonal relationship in social context. However, when a concern regarding mental health status arises, it becomes a serious threat for the individual or to the entire society. The associated result of the mental health issue can be disastrous most especially at adolescence and adulthood [1]. Based on Sommers’ survey [1], the effect of hearing loss on mental health among individuals with hearing loss becomes evident when disability starts effecting the communicative skills which in turn becomes a serious concern. Hearing loss basically includes those who group of individuals who are Deaf and/or Hard of hearing. In other words, the inability to perceive or comprehend any kind of auditory/verbal stimulus as compared to individuals with normal hearing ability has an extensive impact on psychosocial development of individuals with hearing loss. The most crucial effect in the life of an individual with hearing loss is incompetent to follow verbal instructions, and this limits the potentiality to develop speech and language skills which is the essential for communication thus having a cascading effect every aspect of human life including emotional and social development, family interconnectedness, social competence and over all perceived quality of life [2]. Current research studies indicate that persons with hearing impairment tend to exhibit more behavioural and social problems as compared to normal peers [3,4], they frequently experience a greater deal of psychosocial challenges with reduced satisfaction, lack of interests in physical and other recreational activities [4]. Individuals with varying types of hearing loss also tend to show increased rate of being withdrawn or isolated [5,6]. Moreover, in such population access to incidental learning is often confined because of difficulties in communication and the level hearing loss per se. These individuals may often reflect difficulties in cognitive activities like abstract thinking and tasks related to problem-solving [7], ability to form social relationships, very low self-esteem [8] and resulting in high psychological distress causing stress or depression [9]. As mentioned earlier, individuals with hearing loss also have risks related to health and environmental hazards, more prone to maladjustment in social environment, sleep disturbances/insomnia and feasibility of inducing
According to World Health Organization [11], depression is regarded as a serious mental condition which affects an individual with notable depressed mood, displeasure, feelings of guilt and reduced self-worth, decreased energy, disturbed sleep, loss of appetite, and poor concentration. Additionally, there is a close relationship between symptoms of anxiety with depression which could result in substantial comorbid conditions that may negatively influence on everyday responsibilities. Studies have also revealed that slowed responses, tearfulness, loss of appetite, as well as sleep problems, loss of interest or societal withdrawal from family and friends are indicative of depressed individual with hearing loss [12]. Depressive disorders at adult stage is considered as a precursor from the most susceptible age range especially during adolescence [13,14]. Kim-Cohen et al. [15] conducted a study among 1,037 individuals who had history of depression and results indicated that only 25% of participants had suffered from depression at adulthood while 75% of adults who met the criteria for major depression, had an significant history of depressive disorder in childhood or adolescence. A similar kind of study was conducted by Moffitt et al. [16], which revealed that the prevalence of major depressive disorders ranges from 10%-17% in early adulthood period with more depressive symptoms observed in women as compared to men [17]. In other words, symptoms of depressive disorders starts to evolve between 4-5% during early teenager age period especially more common in girls due to the pubertal physical reformation which is much self-evident than in boys [18]. Various research studies also state that incidence of psychopathology in children and adolescents tends to be higher depending on the various degrees of hearing loss [19]. But still, there is still controversial discussions as there in lack of studies that can mention the exact age period of depression as other factors associated with depressive symptoms among adolescence seems vary from individual to individual [20,21]. According to World health Organization [22] depression is one of the leading causes of disability with a 50% higher rate among women than men. It also co-exists or emerge due to other disabling conditions for persons with hearing loss. Research studies also indicate that individuals with hearing loss most especially African Countries Individuals with hearing loss suffer more from depression and psychosocial issues [23], poor academic achievement [24,25], delay in speech and language acquisition [26]. Based on the fact that individuals with hearing loss are more susceptible to having mental health problems due to their inability to communicate with the hearing world. This review study aims to determine the extent of studies which are being conducted on depression and depressive symptoms among persons who are suffering from hearing loss which are based on the open access. Moreover, this study will provide an insight on the regarding the impact of hearing loss on mental health among persons with hearing loss across various countries.
Method
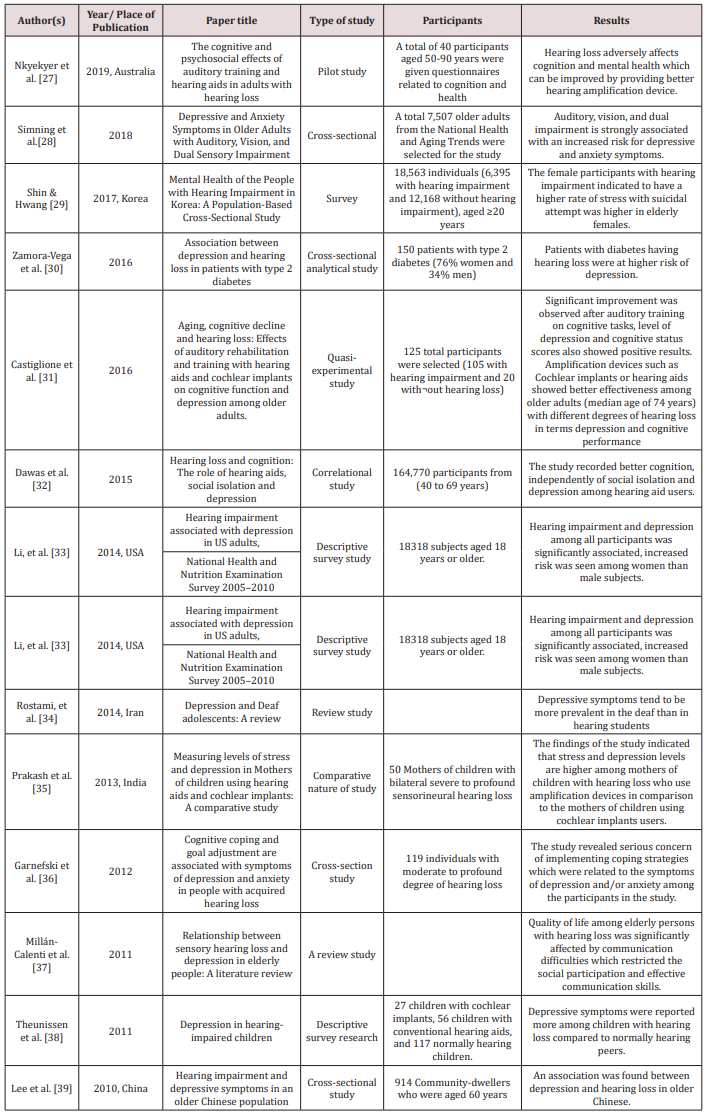
A comprehensive review of articles on ‘depression’ and ‘hearing loss’ or hard of hearing and/or deafness reflected in respective research title were identified and considered for the selected study. However, such article must be completed and published from 2010 up to May 2019. The studies incorporated in the present review were identified by keyword searches from various database sources like PubMed data, Science Direct, and the widely accepted web using Google Scholar. Only those articles which were written in English language was identified and analysed for the current study [27-39]. The search was also extensively done by include other expandable keywords like ‘depressive symptoms’ and ‘Mental Health and Deafness’, ‘Effect of depressive symptoms and Onset of hearing loss’. A The relevant articles searched and considered are presented below (Table 1).
Table 1: MRI of the parotid gland showing homogeneous mass on the superficial lobe of the left parotid gland on hyper signal T1 and T2 and a weak signal on fat suppressed sequences. The lesion is hypointense to parotid and uniformly non-enhancing.
Discussion
Hearing loss is a hidden disability that has an immense negative impact in the quality of life among individuals of any age group from neonates to older adults. Hearing loss irrespective of any degree or configuration plays a role in compromising acquiring communication skills, education, social functioning of the individual. It is the greatest handicap which revolves around the development of speech and language skills; however, because hearing loss is a masked disability, it often neglected, when associated health issues are also present. It may have hazardous effect for overall development of an individual [40]. Oyiborhoro concluded in the study that the difficulties faced by children with hearing loss can extend beyond the academic area which can interfere in the entire social and emotional development resulting in various emotional which can persist even till adulthood [41]. Studies have also indicated that persons with hearing loss found often tend to face situations related to physical abuse, illness or additional disability, as well as feeling withdrawal or isolation from family [42-44]. This review was conducted to highlight the trend of research and trace the effect of hearing loss on depression on individuals with hearing loss. The review also throws light on the associated factors which predispose the depressive symptoms among the Deaf and/or hard of hearing that may lead to suicidal attempts among persons with hearing loss. Hence, when planning an intervention programme for a person with hearing loss should consist of a team which must include audiologist along with psychologist, psychiatrist, sign language interpreters and other professionals. In future, various other similar studies can be conducted by other professional dealing with mental health research and should beam the light on depressive symptoms among persons with hearing loss. Such future studies should also consider the various diversities among persons with hearing loss that will provide the actual evidences and also provide an insight on the prevalence of depression and its symptoms among persons with hearing loss across the world. Apart from these evidences, studies should also focus more on children and adolescents with post-lingual hearing loss while audiologist and the entire team consisting of psychologist should not presume or infer any depressive symptoms among persons with hearing loss without proper intervention.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/
Lupine Publishers: Lupine Publishers | Injuries to Ear Ossicles
Friday, October 16, 2020
Lupine Publishers: Lupine Publishers | Bilateral Dens in Dente in Max...
Lupine Publishers | Lipoma of the Parotid Gland: A Case Report
Lupine Publishers | Journal of Otolaryngology
Abstract
Lipoma of the parotid gland is extremely rare, accounting for only 0,6% - 4,4% of all parotid tumors. We present a rare case of lipoma of the superficial parotid lobe. A 68 - year-old man, presented in our department with a mass of the left parotid region. Clinical examination revealed a mobile, soft, non-tender mass in the area of the left parotid gland. MRI concluded to a lipoma of the superficial lobe of parotid gland. Parotidectomy preserving the facial nerve was performed. No complication nor recurrence were noted after a follow-up of 12 months. Lipoma arising in the parotid gland is extremely rare. Resection of this tumor requires full exposure of the facial nerve and its branches.
Keywords: Lipoma; Parotid gland; Superficial lobe; Parotidectomy
Introduction
Lipoma is a common mesenchymal soft tissue tumor that can be found in any part of the body. It can develop in the head and neck region in 15–20% of cases. Rarely it can arise in the Parotid gland with a ranging incidence from 0,6 to 4,4 % [1]. Clinical diagnosis may be difficult. MRI is necessary, in diagnosis [2]. Surgical management of these tumors is challenging and need meticulous dissection of the facial nerve. We report a case of lipoma arising of the parotid gland and we discuss through literature its clinical and therapeutic features.
Case Report
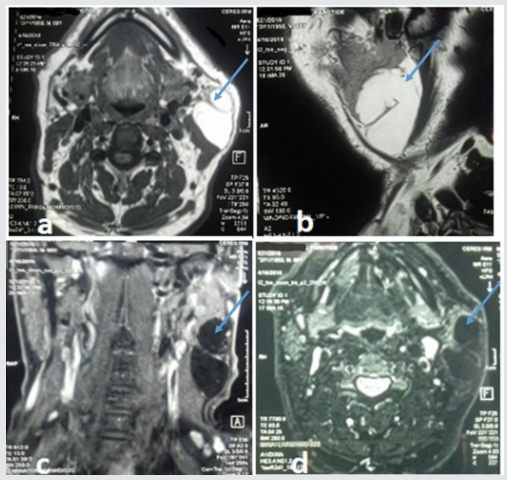
A 68 - year-old man presented with mass of the left parotid region, which was painless slow-growing for 5 years. Clinical examination revealed a mobile, soft, non-tender mass that measured about 6cm in diameter in the area of the left parotid gland, extending from the ear lobule to the left mandibular angle. There was no facial paralysis nor evidence of cervical lymphadenopathy. Magnetic resonance imaging (MRI) showed a well-defined homogeneous lesion of the superficial lobe of the left parotid gland with an enhanced signal on T1- and T2-weighted sequences and weak signal on fat suppressed sequences (Figure 1). The diagnosis of intra parotid lipoma was evoked. A left superficial parotidectomy preserving the facial nerve was performed. The specimen was soft, yellowish, well- circumscribed measuring 80*34mm. Histological examination revealed a well-circumscribed aggregate of mature adipocytes surrounded by a thin fibrous capsule confirming the diagnosis of intraparotid lipoma. No recurrence or complication were observed after a follow-up of 12 months.
Discussion
Lipoma is one of the most frequently encountered benign mesenchymal tumors that may originate from adipose tissue in any part of the body [3,4]. Rarely, it can develop in the parotid gland with reported incidence ranging from 0,6% to 4,4% among parotid tumors [3,5]. Lipoma may occur at any age, but most frequently between 40 and 60 years with a male predominance [5,6]. Its aetiology is unknown. It can be caused by heredity, obesity, diabetes, radiation, endocrine disorders, insulin injection, corticosteroid therapy and trauma [7]. In our case, we did not find any aetiological factors. Most of the reported cases were located at the superficial parotid lobe [7]. Lipomas involving the deep parotid lobe are extremely rare [5-8]. Clinical diagnosis may be difficult [9], especially for tumors located at the deep parotid lobe because it is difficult to evaluate the relationship between these masses and the surrounding tissues. Those situated at superficial parotid lobe usually appear as a slow growing, non-tender, movable and well-differentiated soft mass in parotid region [3-10]. Facial paralysis and pain are uncommon signs and rarely have been described [5-11]. This benign clinical presentation is most often mistaken for Warthin tumor or pleomorphic adenoma [3-12]. Fine needle aspiration cytology (FNAC) has great value in the diagnosis of parotid tumors and requires an experienced cytologist. Its accuracy drops to less than 50% in the cases of parotid lipomas [5-13]. On imaging, CT scan shows hypodense, homogeneous and well delineated mass with few septations and negative attenuation, without contrast enhancement [3-13]. However, CT scan cannot distinguish lipoma from surrounding adipose tissue. MRI remains the best diagnostic tool that can accurately diagnose lipomas [5-1]. Lipomas produce strong signals on T1- and T2 weighted sequences and weak signals on fat-suppressed sequences. After Gadolinium injection, the mass still hypointense to parotid, homogeneous in signal and uniformly non-enhancing [3]. MRI can also clearly define the limits of lipoma from normal adipose tissue and may be useful in determining the appropriate surgical approach.
Figure 1: MRI of the parotid gland showing homogeneous mass on the superficial lobe of the left parotid gland on hyper signal T1 and T2 and a weak signal on fat suppressed sequences. The lesion is hypointense to parotid and uniformly non-enhancing.
Histopathologic investigation reveals mature adipose tissue separated from parotid gland parenchyma with a fibrous capsule. Identification of a capsule may aid in distinguishing such a neoplasm from pseudolipoma, lobular lipomatous atrophy, or lipomatosis, all of which are unencapsulated [3]. Surgery is the treatment of choice of parotid gland lipoma, but its modalities remain controversial [8-12]. It should be performed by experienced surgeons because of the need for meticulous dissection of the facial nerve branches. The postoperative esthetic and functional results should be the major concerns [1]. Some surgeons recommend simple enucleation of a superficial lobe parotid lipoma with a small border of healthy parotid gland parenchyma, as this is easy to perform because of the well-defined capsule. Other surgeons suggest that the surgical management of parotid lipoma should be the same as that for other parotid tumors [5]. However, it is well known that transient facial nerve dysfunction and Frey’s syndrome may occur as complications following surgical intervention for parotid tumors and should be explained to the patient before operation [5]. Facial nerve dysfunction ranged between 8.2 and 65% after parotid gland surgery for benign tumors [10]. Therefore, it requires efforts such as facial nerve monitoring to identify the facial nerve. Recurrence rate of parotid lipoma after adequate resection is very low. It has been reported in 5% in all cases when it is well-encapsulated [5-9]. Malignant transformation into liposarcomas has been reported in few cases in the literature [9]. Therefore, careful follow-up is recommended.
Conclusion
Lipoma of the parotid gland is a rare benign tumor, which should be considered in the differential diagnosis of parotid gland’s mass lesions. MRI is essential to locate the tumor, and to precise its relationship with the facial nerve. Their management is challenging. Definitive diagnosis can only be accomplished with histopathologic review.
Read More Lupine Publishers Otolaryngology
Journal
Articles:
https://lupine-publishers-otolaryngology.blogspot.com/
Read More Lupine Publishers blogger Articles:
https://lupinepublishers.blogspot.com
Choanal Atresia Repair, A Comparison Between Transnasal Puncture With Dilatation And Stentless Endoscopic Transnasal Drilling
Abstract Background: in this study we present the outcome of surgical repair of choanal atresia of 33 patients underwent t...