Monday, July 29, 2019
Lupine Publishers: Interior Environmental Design, Heal? | Lupine Publ...
Lupine Publishers: Interior Environmental Design, Heal? | Lupine Publ...: Open Access Journal of Complementary & Alternative Medicine | lupine Publishers Abstract Osteoporosis is a largely p...
Wednesday, July 24, 2019
Lupine Publishers | Oral Health Status in Children with Autism Spectrum Disorder Presenting in Yaoundé, Cameroon
Lupine Publishers | Journal of Otolaryngology
Abstract
Introduction:
Children with Autism Spectrum Disorders (ASD) present with a lifelong
neuro-developmental disorder that makes them prone to oral diseases. The
aim of the present study was to describe the oral health status of
children with ASD attending autism centers of Yaoundé, Cameroon.
Methodology:
A descriptive cross-sectional study was conducted in seven specialized
centers caring for children with autism. A structured questionnaire and
clinical examinations were used to collect the data.
Results:
Ninety six children aged between 3 to 14 years, the majority of whom
were boys (80%), were recruited into the study. The majority were from
kindergarten (75%) and the remainder primary schools. Tooth brushing for
most of the children (71%) was carried out by their mother. Half of the
children brushed once a day with the help of their mothers usually in
the morning before breakfast, using toothbrushes and toothpaste. Most of
the children consumed soft and sweet diets that included sweetened
fruit juices and had never been to a dentist. The prevalence of caries
was 66.13%. Dental caries was more pronounced in the 7 to 11 year old
age group. Almost half (45.21%) had gingivitis associated with plaque
and calculus and 59.19% had gingival bleeding. The prevalence of trauma
to both hard and soft oral tissues was 45.83% while the prevalence of
dental abnormalities was 31%. The treatment needs of the children
include dental fillings, scaling and curettage.
Conclusion:
Children with ASD presented with a high prevalence of dental caries and
periodontal diseases, bad breath and dental trauma to hard and soft
tissues.
Recommendation:
Since autism patients present with many functional and clinical
problems, a multidisciplinary approach is needed in Cameroon for the
management of medical, dental and behavioral problems.
Keywords Autism Spectrum Disease; Cameroon; Children; Oral health
Introduction
Oral
diseases such a dental caries and periodontal disease are the most
common chronic diseases and are important public health problems because
of their high prevalence [1]. Oral health and general health are
interlinked, affecting and affected by one another. General health can
affect oral health. Medical conditions often have oral implications and
consequences [1,2] and one disease affecting general health that can
affect oral health is Autism which is considered a disease of special
care within the oral health care services. Results of the 1994–1995
National Health Interview Survey of the USA on access to care and use of
services indicated that the most prevalent unmet health need among
children with special health care needs was oral health care [3]. During
the 2014– 2016 survey, the prevalence of children aged 3–17 years who
had ever been diagnosed with a developmental disability increased from
5.76% to 6.99%. During this same time, the prevalence of diagnosed
autism spectrum disorder and intellectual disability did not change
significantly. The prevalence of autism spectrum disorder, intellectual
disability, other developmental delay, and any developmental disability
was higher among boys when compared with girls [4]. Autism spectrum
disorder (ASD) is a persistent neurodevelopmental condition with early
childhood onset. It begins in early childhood and persists throughout
adulthood affecting three crucial areas of development: communication,
social interaction, and creative or imaginative play [5]. The universal
occurrence of autism spectrum disorders (ASD) was investigated about
twenty-six years ago and it was thought to occur only in western
industrialized countries that had high levels of technological
development.
Over
the years, knowledge about ASD and its prevalence has been documented
as being on the rise in different regions of the world, with most
literature coming from the western world, while the situation in Africa
remains unclear [5]. No specific oral manifestations of ASD have been
described, although the oral hygiene is known to be deficient [6].
Nevertheless, many authors have found the prevalence of caries and of
periodontal disease to be no different compared with non-autistic
individuals [6] and in some cases the prevalence of caries in children
with ASD may even be comparatively lower [6]. Between 60–95% of all
patients with ASD have an unusual sensory profile, including dysfunction
in registering oral sensitivity. Studies have shown a high prevalence
of periodontal and orthodontic problems such as crowding of the
dentition in children with autism as compared to non-autistic children
[7,8]. In addition, systemic medications taken by autistic patients may
also affect their oral health. It has been reported that nearly 25% of
young people with ASD present with gingival hyperplasia related to
antiepileptic medications. Furthermore, some medication may compromise
the health and function of the oral environment causing decreased
salivary flow, dry mouth and a reduced mechanical and antibacterial
action of saliva [8]. In recent years, there has been an increasing
awareness of autism and autism-related diseases in the Cameroon.
However, there is a paucity of information regarding the oral
manifestations and the oral health care needs of children with ASD. The
aim of the present study was to determine the prevalence of the oral
manifestations in autism patients and to establish their oral health
needs.
Methodology
This
descriptive study was carried out in Yaoundé between January to July
2017 in all the specialized centers taking care of children with autism.
These centers currently take care of children with ASD aged between
3–14 years regardless of gender. The eight centers identified were in
five districts of the city of Yaoundé. Outside the Center for Special
Education for children with ASD located in the district of Yaoundé I,
the target population consisted of 145 children in four districts of the
city of Yaoundé (II, IV, V, and VI). The districts of Yaoundé III and
VII lacked education centers. Of the eight identified centers, seven
agreed to participate in the study from the 4 districts based on the
approval or consent of parents or guardians. Children aged between three
and fourteen years old were included in the study. The inclusion
criteria for participation in the study were defined before the sample
were screened and consisted of the following: a diagnosis of ASD, the
understanding of very simple instructions and written informed consent
from the parents or caregivers. Data collection began following the
approval by the relevant authorities as well as the consent from the
parents and caregivers of the participants. Information from the
patients was collected using a data capture sheet after which clinical
examinations were carried out on a mobile dental clinic under bright
natural light. The parents / caregivers of the participants received an
explanation of the study, together with an information sheet and
informed consent form. Those who agreed to participate completed a
questionnaire evaluating the socio-demographic status of the children,
medical history, functional disabilities, nutritional status,
nutritional habits and oral hygiene of the patients. Data not adequately
recorded were obtained by interviewing the parents or caregivers.
A
single dentist was used to carry all the clinical dental examinations
using a mirror and probe on a portable dental chair and guidable light
source of enough power for adequate intraoral exploration. At the end of
the examination, the parents and caregivers received a report on the
oral disorders found, with suggestions for referral regarding the
necessary treatments and dental care. Clinical examinations were carried
out to evaluate the oral health status, the prevalence of dental
caries, periodontal diseases, enamel hypoplasia, hard and soft tissues
trauma and other pathologies in the oral cavity. The DMFT index was
determined assessing the decayed, missing and filled teeth. Oral hygiene
was rated using the Simplified Oral Hygiene Index (OHI-S). The criteria
of this index are related to the sum of the Plaque Index Score (PI-S)
and the Calculus Index Score (CI-S). In both cases the surfaces of index
teeth were examined: vestibular surfaces of 11, 16, 26 and 31; lingual
surfaces of 36 and 46. In the absence of index teeth, the entire sextant
was recorded to the maximum degree (except for the third molars).
Statistical Analysis
Data
were captured into Microsoft excel 2010 and exported to SPSS for
statistical analysis. Results were presented in the form of tables using
Microsoft Excel 2010. Bivariate analysis was carried out using
Chi-square test for qualitative variables and ANOVA for quantitative
variables p= 0.05.
Ethical Considerations
Approval
to carry out this study was obtained from the Ethics Committee of the
University des Montagnes. Informed consent was obtained from parents and
all information obtained was strictly confidential. Participants were
informed that they were free to leave the study at any stage without
penalty to their further management.
Results
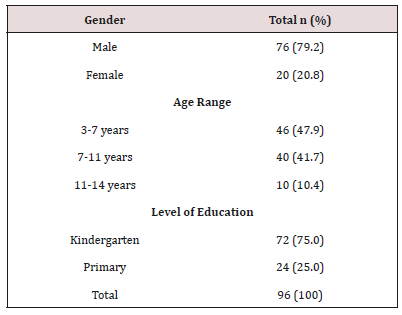
The
sample consisted of ninety six children aged between 3 to 14 years.
More than two thirds were male. Almost half 46 (47.9%) were in the
3–7year age group while a more than a third 40 (41.7%) were in the 11–14
year old age group. Children in Kindergarten were most represented
(Table 1).
Table 1: Socio-Demographic Characteristics.

Distribution of Bacterial Plaque and Gingivitis
Large
amounts of dental plaque deposits were found in half (45.21%) of
children 3 to 7 years and 44.41% between the ages of 7 to11 years had.
Distribution of Dental Pathologies
Gingival
bleeding was found in 59.19% of the 7–11 year old children, 55% in 3–7
year old’s and 16.14% in the 11–14 year old children. Two thirds
(66.13%) of children aged between 7 and 11 years presented with dental
caries Crown fracture (58.33%) was found in more than half of the
children aged between 3 and 7 years. Overall the mean DMFT index was
2.76, the plaque index was 3.91 and the gingival bleeding index 2.32.
Enamel opacities were found in 51.43% in children aged 3 to 7 years,
45.71% aged between 7 and 11 years and 2.86% in the 11–14 year old
children). Enamel hypoplasia was identified in 42.86% in children aged 3
to 7 years, 50% in those between 7 and 11 years and 7.14% in the 11–14
year old children. Macrodontia was found in 71.43% in children aged
between 11 and 14 years) compared to 28.57% in those aged between 7 and
11 years. Orthodontic problems like malocclusion and crowding was found
in 9.37% of the children. The prevalence of trauma to dental soft
tissues was 45.83% while the prevalence of dental abnormalities such was
31%. Nutritional practices, oral hygiene practices and oral health
seeking behavior. More than two thirds (62.5%) of the children were
exposed to cariogenic foods. Tooth brushing for the majority (70.83%) of
the children was carried out by their mother. Half of the children
brushed once a day. The majority brush their teeth before eating in the
morning. Only 3 children brushed in morning and evening after meals. Two
children reported brushing morning, afternoon and evening after meals.
Only 13.54% had ever visited a dentist. Almost all 95.8% of the children
had problems with word pronunciations. More than a third 38.5% of the
children had difficulties talking aloud, a quarter had inconsistent
speech (25%) and a quarter with incoherence when singings 20.8%. More
than three quarters (80.2%) of the children presented with dental
sensitivity (Table 2). Almost all 93.8% the children were not satisfied
with their diet, 64.6% had difficulty with food intake (meals) and 62.5%
avoid eating (Table 3).
Table 2: Functional Disorders.


Table 3: Dietary Behaviors.


Discussion
Autism
spectrum disorders (ASDs) comprise a complex set of related
developmental disorders that are characterized by impairments in
communication, social interaction, and repetitive behaviors. Impairments
in sensory processing are also very common. The prevalence of ASD is
increasing and is currently estimated to affect 1 in 150 children
worldwide [9]. It has been documented in many areas of the world that
ASD is dominant among male children (3,4,5,6) as was found in the
present study where there was a predominance of male children presenting
with ASD. Various studies have reported the male: female ratio to range
from 2:1 to 16:1 [9]. However, a recent systematic review carried out
by Loomes R, in which fifty-four studies were analyzed, with 13,784,284
participants of whom 53,712 had ASD (43,972 boys and 9,740 girls)
concluded that the true male-to-female ratio is not 4:1 as is often
assumed but rather, it is closer to 3:1. There appears to be a
diagnostic gender bias meaning that girls who meet criteria for ASD are
at disproportionate risk of not receiving a clinical diagnosis [10].
Whatever the true ratio, clinical referrals to a specialist diagnostic
centre have seen a steady increase in the number of girls and women
referred. Because of the male gender bias, girls are less likely to be
identified with ASD, even when their symptoms are equally severe. Many
girls are never referred for diagnosis and are missed from the
statistics. Emphasis is placed on the different manifestations of
behavior in autism spectrum conditions as seen in girls and women
compared with boys and men [7].
The
age group most represented in the present study population was between 3
and 7 years old. This could be explained by the fact that after the
appearance of the first symptoms during the first three years of life,
either from birth or shortly after 12 months [3]. The kindergarten age
group was more dominant in our study as three quarters of the children
attended kindergarten. This age group is very important in children with
ASD as an important transition period. The kindergarten transition is
the first major educational transition in a child’s educational career.
It is a particularly important transition for those with ASD because a
successful kindergarten transition leads to better academic outcomes and
better generalization of skills developed in the pre-school setting
[8,9]. However, children with ASD begin with significant risk of an
unsuccessful transition to kindergarten due to qualitative impairments
in social communication and behavior. The use of recommended practices
in kindergarten transition increases the chance of a successful
transition for students with ASD [8,9]. Transitions in general, whether
it be from one activity to another or one setting to another, are
difficult for children with ASD [10]. These difficulties are often
characterized by problems such as aggression, non-compliance, tantrums
and a lack of consistent participation in activities [10]. It is because
of these difficulties that the management of ASD is carried out using a
multidisciplinary approach. The most effective strategies being based
on educational programs [6,10]. In order to educate children with ASD,
it is necessary to facilitate structured situations helping the patients
to anticipate what is going to happen [6], since they show great fear
and anxiety in the face of unknown situations [6], such as visiting the
dental clinic. The dental care of these patients poses great
difficulties, and in most cases, treatment is provided under general
anaesthesia [6,11–16].
Eating Habits and Oral Hygiene of Children ASD
ASD
are a major health and educational problem affecting many areas of
daily living including eating. Children with ASD are often described as
picky or selective eaters [12]. This was confirmed in the present study
as two thirds of children preferred a soft and sweet diet. Poor reflexes
during mastication and poor coordination of the tongue prevents normal
swallowing and this results in a tendency to store food in the mouth and
hence a preference for soft food. Various factors may contribute to
food selectivity and several explanations have been proposed [12]. One
of these factors relates to sensory sensitivity (also referred to as
sensory defensiveness or sensory over-responsivity). Ayres [17] first
described sensory defensiveness as the tactile domain (tactile
defensiveness) in some children with learning and behavioral disorders.
She described tactile defensiveness as an over-reaction to certain
experiences of touch, often resulting in an observable aversion or
negative behavioral response to certain tactile stimuli that most people
would find innocuous. For example, children who show tactile
defensiveness often have difficulty being cuddled and pull away from
touch. It is possible that early tactile sensitivity may contribute to
some of the sensory feeding issues such as difficulty with food textures
seen in children with ASDs [12].
Oral Hygiene Status and Practice
The
present study showed that the oral hygiene practices in terms of the
frequency, duration and period of tooth brushing was very poor due to
lack of co-operation, therefore the prevalence of dental caries and
gingivitis is high. Parents and careers reported difficulties when they
brushed the children’s teeth [14] further compounded by the lack of
manual dexterity of autistic children. Morales-Chávez (2017) found a
lack of cooperation in daily dental hygiene in 35.7% of children with
ASD. Maintaining good dental hygiene is a difficult task for 40 to 50%
of people with ASD [15]. Rada (2010) similarly argues that lack of oral
hygiene is one of the biggest causes of rapid increases in caries rates
and periodontal disease in young people with ASD compared to
neurotypical children [16]. In general, children preferred soft and
sweetened foods, and tend to ‘pouch’ food inside the mouth instead of
swallowing it due to poor tongue coordination, thereby increasing the
susceptibility to caries [18,19]. Studies have shown that children with
autism exhibited a higher caries prevalence, poor oral hygiene and
extensive unmet needs for dental treatment than non-autistic children
[19–21] this concurs with the present study where high levels of dental
plaque was found. The children also presented with a high mean DMFT
index, a high plaque index and a high gingival bleeding index and
therefore require stringent oral hygiene practices. In the present
study, oral hygiene practices were carried out mainly by the mothers of
the children.
Vajawat
and Deepika [19] suggested that attempts should be made by parents,
general dentists and periodontists to teach oral hygiene methods to the
children by constant repetition and patience, as autistic individuals
can develop skills over a period and lead a more productive and
independent life [19]. Jaber MA [18] also suggested that oral health
programmed that emphasize prevention should be considered of importance
for children and young people with autism [18]. Another reason for high
prevalence of oral diseases in autism children is poor access to oral
health care facilities. In the present study 86.46% of the children with
ASD never consulted a dentist and this could be due to the lack of
infrastructure and human resources to manage the children in Cameroon.
Bartolomé Villar and colleagues [22] in their review, reported that
certain disorders are more prevalent in association with ASD —
malocclusions, enamel hypoplasia, parafunctional habits (bruxism) and
deleterious habits (mouth breathing, tongue thrusting, rumination) as
well as a higher incidence of dental trauma, owing either to accidents
or to self-imposed injuries [22]. Similarly, in the present study,
dental malocclusion, enamel hypoplasia and enamel opacities were
observed among the children with ASD, as was bad breath. Motta et al.
[23] found a statistically significant association between halitosis and
mouth breathing [23]). In the present study the prevalence of dental
trauma to both the hard and soft tissues was very high as compared to
the case-control study carried out by Altun et al. [24] on ASD children
(AG) and a control group (CG). They reported that the rate of injury was
higher among the AG (23%) than the CG (15%), though the difference
between the 2 groups, however, was not statistically significant
(P<.19). The most common type of dental injury was enamel fracture.
The rate of enamel fracture was higher in the CG (59%) than in the AG
(33%), and the distribution of types of traumatic injury differed
significantly between the AG and CG (P>.01). According to their
study, the maxillary central incisors were most affected and enamel
fracture was mostly common. This is because the maxillary central
incisors are the more prominent and are the first teeth receive impact.
In our study, the high level of injuries might because of the play
grounds, or the surroundings of the children are not protected from
activities that might prevent impactful contacts. In conclusion,
children with autism presented with a high prevalence of dental caries
and periodontal diseases, bad breath, and dental trauma to hard and soft
tissues.
Recommendation
Since
autism patients present with many functional and clinical problems, a
multidisciplinary approach is needed in Cameroon for the management of
both dental and behavioral problems.
For more Lupine Publishers Open Access Journals Please visit our website: h
https://lupinepublishersgroup.com/
For more Journal of Otolaryngology-ENT Research articles Please Click Here:
https://lupinepublishers.com/otolaryngology-journal/
https://lupinepublishersgroup.com/
For more Journal of Otolaryngology-ENT Research articles Please Click Here:
https://lupinepublishers.com/otolaryngology-journal/
To Know More About Open Access Publishers Please Click on Lupine Publishers
Lupine Publishers: The Painful Ischiopubic Synchondrosis: A Case Repo...
Lupine Publishers: The Painful Ischiopubic Synchondrosis: A Case Repo...: Journal of orthopaedics | Lupine Publishers Abstract Van Neck-Odelberg disease is considered a benign skeletal develo...
Monday, July 22, 2019
Lupine Publishers: Lupine Publishers | Advances in Robotics & Mechani...
Lupine Publishers: Lupine Publishers | Advances in Robotics & Mechani...: Journal of Robotics & Mechanical Engineering | Lupine Publishers Smart Robotics for Smart Healthcare Abstract The...
Thursday, July 18, 2019
Lupine Publishers: Surfactant Mediated Biodegradation of Aromatic Hyd...
Lupine Publishers: Surfactant Mediated Biodegradation of Aromatic Hyd...: Journal of Oceanography | Lupine Publishers Abstract Aromatic hydrocarbons (toluene and xylene) are highly water soluble and their...
Friday, July 12, 2019
Lupine Publishers: Lupine Publishers Group
Lupine Publishers: Lupine Publishers Group: Lupine Publishers Group Lupine Publishers is a world’s leading Online Publishing repository, a genuine publisher with quality medical...
Thursday, July 4, 2019
Lupine Publishers: Journal of Veterinary Science- Lupine Publishers
Lupine Publishers: Journal of Veterinary Science- Lupine Publishers: Report of Outbreak of Ruminal Impaction Due to Indigestible Foreign Bodies in Sheep, in Northwest of Iran by Mohammad Reza Mohebbi in C...
Monday, July 1, 2019
Lupine Publishers: Journal of Chemical Sciences-Lupine Publishers
Lupine Publishers: Journal of Chemical Sciences-Lupine Publishers: Biological Studies, Synthesis, Structural, Spectral Characterization and Co-Ordinate Mn (II), Fe (II), Zn (II) (II) Complexes Containing ...
Subscribe to:
Comments (Atom)
Choanal Atresia Repair, A Comparison Between Transnasal Puncture With Dilatation And Stentless Endoscopic Transnasal Drilling
Abstract Background: in this study we present the outcome of surgical repair of choanal atresia of 33 patients underwent t...
